CMS Interoperability and Patient Access Final Rule Requires a Robust Patient Identification Software

This has been quite a year for the U.S. healthcare system – nobody could’ve predicted all the series of events. While the novel coronavirus is still raging on, telehealth is experiencing unprecedented growth. On the other hand, hospitals are facing immense financial strain due to the pandemic’s consequences such as the cancellation of elective procedures and lower inpatient visits. However, despite all the recent developments healthcare providers need to work on something else as well – supporting e-notifications. CMS has made some additional changes to the Medicare Conditions of Participation (CoPs), and while providers will be busy brainstorming about how to best approach the requirements, many will overlook one critical factor that will either make or break their e-notifications – patient identification. Let’s take a look at what the rule specifically says about e-notifications, who is eligible, how it helps caregivers, and how a robust patient identification software like RightPatient is a must for ensuring proper e-notifications.

The Interoperability and Patient Access Final Rule – in a Nutshell
While the rule itself is quite vast and detailed, we’ll cover the e-notifications part briefly. The basic meaning of the rule is clear from its name. For years, the U.S. healthcare system has been suffering from the lack of proper interoperability for a number of issues – patient misidentification being a major reason. However, with the “companion final rule”, as per CMS, things are about to change for the better, as it will introduce a certain level of interoperability that will ultimately boost coordinated healthcare efforts.
The “companion final rule” states that healthcare providers such as critical access providers, acute care, or psychiatric hospitals must send out real-time e-notifications during ADT (admission, discharge, or transfer) events to a patient’s caregivers such as established primary care practitioners, post-acute providers & suppliers, primary care practice groups & entities, as well as any other practitioners, groups, or entities primarily responsible for the patient’s care. The information sent must contain the patient’s name, the treating practitioner’s name, and the sending institution’s name, at the very least. Finally, these are applicable during inpatient ADT events and ED admissions or discharges.
Any caregiver that uses digital medical records such as EHRs or EMRs must support e-notifications by May 1, 2021, to ensure CMS compliance.
With that out of the way, let’s look at how the rule requires accurate patient identification and how a robust patient identification software is critical for its success.
Why patient identification will make or break your CMS compliance
Healthcare providers are already busy working on e-notifications support, and while there are a lot of great solutions out there, providers shouldn’t forget the foundation upon which e-notifications depend on – proper patient identification.
The Interoperability and Patient Access Final Rule requires hospitals to identify their patients accurately across the care continuum, especially if they want to send out e-notifications to the proper caregivers. Sadly, patient identification has always been problematic – it is an overlooked but significant concern for the U.S. healthcare system. One might ask how are patient identification and e-notifications related – let’s learn more.

Imagine this – a hospital already has patient misidentification cases because they don’t use an effective patient identification software. If a patient comes in and is misidentified, not only will the treatment be affected, but the hospital will be sending out false alerts to the wrong caregivers. This will wreak havoc for all the caregivers involved with the patient.
If such cases become common, then the patients, as well as the care coordination teams, will start questioning the credibility of the caregiver sending out false alerts. As a result, the hospital will lose goodwill and risk its CMS reimbursements. After COVID-19, not a single hospital can afford to make such mistakes – the pandemic has already caused the worst financial strain on hospitals and health systems in recent times. Thus, patient identification is a crucial component for the e-notifications to work. If caregivers don’t have a robust patient identity matching system in place, they need to upgrade it before the e-notifications support deadline.
RightPatient is the most robust patient identification software
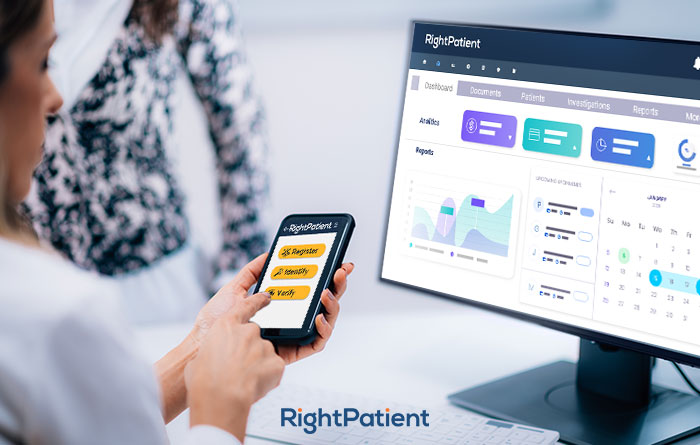
RightPatient has been accurately identifying patients for years. With its touchless patient identification platform, RightPatient ensures that patients are identified accurately and safely right from the start.
After a patient schedules an appointment, they are sent an SMS or email and are required to provide a selfie and a photo of their driver’s license. The platform automatically matches the photos and remotely ensures patient identification. If it’s a new patient, the platform will automatically assign new biometric credentials for them.
During hospital visits, patients only need to look at the camera – RightPatient matches the saved photo with the photo taken by the camera – ensuring accurate patient identification. Best of all, it’s an entirely touchless process, something that is mandatory in a post-pandemic world.
RightPatient is the leading patient identification software in the healthcare industry and is used by prominent caregivers such as Terrebonne General Medical Center, Community Medical Centers, and Catholic Health Services of Long Island. Be a responsible healthcare provider and upgrade your patient identification system now to prevent misidentification cases, medical identity theft, and ensure compliance with the Interoperability and Patient Access Final Rule.





























 Patient data protection has been one of the oldest and most important requirements for healthcare providers, and rightfully so – a patient shares critical and sensitive information with their caregivers. Names, Social Security numbers, dates of birth, contact information, addresses, facial photographs, medical history, and ailments are just some examples of the information stored within patient records. If these get compromised and land in the wrong hands, such cases can have disastrous consequences – healthcare insurance fraud, litigation costs for providers, and hampered patient safety are some common results. Thus, protecting patient data is crucial for any caregiver. Let’s take a look at a few more reasons why protecting patient data is necessary for hospitals and health systems.
Patient data protection has been one of the oldest and most important requirements for healthcare providers, and rightfully so – a patient shares critical and sensitive information with their caregivers. Names, Social Security numbers, dates of birth, contact information, addresses, facial photographs, medical history, and ailments are just some examples of the information stored within patient records. If these get compromised and land in the wrong hands, such cases can have disastrous consequences – healthcare insurance fraud, litigation costs for providers, and hampered patient safety are some common results. Thus, protecting patient data is crucial for any caregiver. Let’s take a look at a few more reasons why protecting patient data is necessary for hospitals and health systems.

 Protecting patient data is a huge challenge, but it is achievable. One of the first and foremost things providers can do to protect patient data is to ensure positive patient identification at each encounter. That’s where we can help.
Protecting patient data is a huge challenge, but it is achievable. One of the first and foremost things providers can do to protect patient data is to ensure positive patient identification at each encounter. That’s where we can help.