Patient Safety and Quality Can Be Improved by Preventing Duplicate Medical Records

Patient safety is one of the more integral aspects of any given healthcare system. It ensures that patients are getting the required treatment without any medical errors or harm, healthcare outcomes are optimal, and healthcare services are delivered to the highest possible standard. While those are the common aims, the reality is quite different in the U.S. healthcare system. It has always been inundated with a number of serious issues – healthcare data breaches, medical identity theft, patient identification issues, lack of price transparency, and duplicate medical records are just some of them. The root cause of many of the issues are duplicate medical records. While we already had a closer look at duplicate medical records and how it impacts revenue cycle optimization, let’s have a look at how preventing duplicates can lead to enhanced patient safety and quality, among other things.

How duplicates impact patient safety and quality of healthcare
In a previous article, we’ve already seen how medical record errors like duplicates and overlays are created and how they cause claim denials. Let’s see how they impact patient safety and quality of healthcare as well.
AHIMA’s Shannon Harris and Shannon H. Houser stated in an issue of the Journal of AHIMA that duplicates and overlays don’t only cause financial woes, but lead the physicians and healthcare staff to inadvertently causing medical errors. For instance, imagine that a single patient has duplicate medical records in a hospital’s EHR system. While treating the patient, the physician will see the duplicates but chooses the one that has obsolete information. Since the information is not updated, the treatment or medication might very well cause adverse effects. Such cases might even lead to transferring the patients for emergency treatments, leading to jeopardized patient outcomes.
That’s not the only way duplicate medical records impact patient safety and quality of healthcare – let’s look at the latter. When you have fragmented information within duplicate records, issues such as repeated lab tests and delays in treatment are quite common. Since the majority of the healthcare providers’ registration systems have ineffective patient identity matching techniques, the number of duplicates keeps on increasing, leading to patient safety issues, patient data corruption, and financial troubles in the form of denied claims.
How are hospitals addressing duplicates?
Sadly, rectifying duplicates and overlays are quite complex and a nightmare for any given healthcare provider. While most of the hospitals are trying to fix duplicates by reallocating their HIM resources and even dedicating some of their FTEs (full-time employees) to identify and rectify the erroneous records, unless they address the frontend issues (read: identify patients accurately), it will be a never-ending cycle. Patients will be misidentified, duplicates will be created, and FTEs will be assigned to fix them on the backend, taking up valuable time and resources.

So, can hospitals address these issues and prevent duplicate medical records on the frontend?
RightPatient enhances patient safety and quality of healthcare
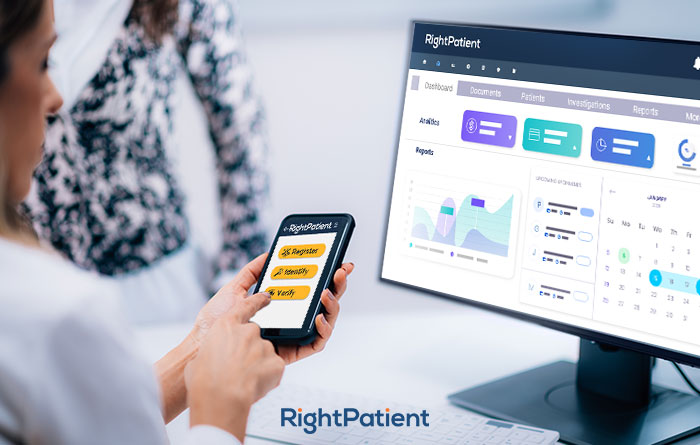
As previously mentioned, if the patients are accurately identified during the registration process, duplicates can be prevented right from the beginning. That’s what we do best with our industry-leading patient identification platform. RightPatient, with its touchless design, ensures that patients are identified across the care continuum, starting from appointment scheduling. Patients only need to provide their selfies and a photo of their driver’s license when they schedule appointments. RightPatient matches the photos and makes sure that the accurate patient record is identified every time the patient accesses healthcare services, remotely or otherwise.
When the patients arrive at the hospital, all they need to do is look at the camera – RightPatient matches the saved photo and the real-time photo during the check-in process, preventing duplicates, eliminating denied claims, and enhancing patient safety. The best part of RightPatient is that the entire identification process is touchless, creating a safe environment for all involved in a post-COVID-19 world.