Patient Identification Policy Impacts Data Integrity and Patient Safety Issues

Let’s face it – patient identification errors are nothing new and it is a much-discussed topic among healthcare leaders. For instance, just a month ago, a new coalition was formed to urge Congress to develop a UPI (unique patient identifier) to be used nationwide. Sadly, such formations are quite common – groups, competitions, and alliances have formed for years for the same reason. The result is that no UPI exists yet and patient identification errors are still wreaking havoc. However, many healthcare providers are reaping the benefits of accurate patient identification – it boils down to the patient identification policy used by the caregiver. Let’s take a closer look at how patient identification errors can cause a multitude of problems, why accurate patient identification is so crucial, and how platforms like RightPatient can help ensure just that.

Patient misidentification
It is quite self-explanatory. Patient identification errors occur whenever a healthcare facility fails to accurately match the patient with their appropriate medical record present within the EHR system.
It happens for a number of reasons. As already mentioned, it is nothing new and has been the result of years of human errors and improper patient data maintenance like duplicate medical records, overlays, and missing, incorrect, and/or incomplete information, leading to low patient match rates.
To put it into perspective, AHIMA stated that health systems can house up to 20% duplicate records within their EHR systems. The financial impact? It can go as high as $40 million for any given healthcare facility.
Effects of patient misidentification
Low patient match rates is just the tip of the iceberg! Patient misidentification leads to several problems. Let’s look at the more prominent effects of patient misidentification.

Whenever you incorrectly identify a patient, it means that one patient’s data will get written into someone else’s medical record – creating patient data integrity issues. This leads to a lot of problems – incorrect medications, repeated lab tests, incorrect medical procedures, inaccurate patient history – the list just goes on. Both the patients will receive inaccurate care by the caregiver as a direct consequence of patient misidentification, hampering patient outcomes.
Naturally, patient misidentification leads to patient safety issues – these are bound to happen if your treatment is based on the wrong medical record. Consequences can be delays in treatment, worse patient outcomes, irreparable damages, and sometimes, patient misidentification can even result in deaths. According to a report by John Hopkins University, medical errors can cause up to 250,000 avoidable deaths per year, many of which happen due to patient identification errors.
Thus, the million-dollar question is how can healthcare providers ensure accurate patient identification across their facilities?
It depends on a provider’s patient identification system
The accuracy of patient identification is as good as the patient identification policy used by the hospital in question, and there are many options hospitals can choose from. Responsible leaders, in any case, must choose the patient identification system that ensures accurate patient identification, provides a seamless experience, and provides a safe and hygienic environment for all involved.

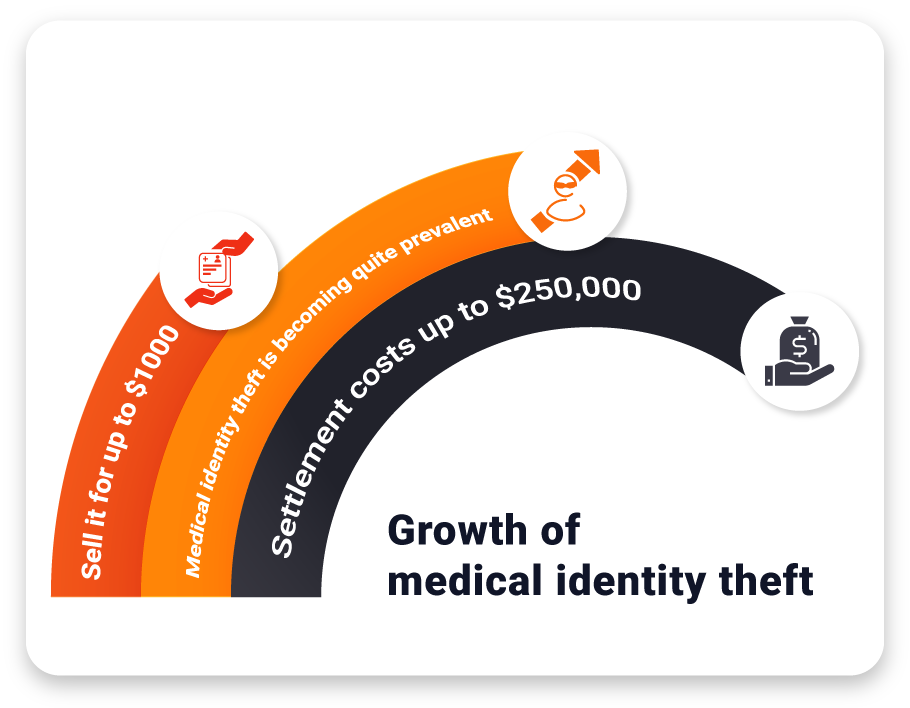
There are a plethora of options available that hospitals can use as their primary patient identification policy. Sadly, many are still choosing the most obsolete one – inundating patients with questions. Whenever a patient arrives, officials ask them questions to find the correct medical record. This policy is slow, outdated, and extremely insecure – anyone can pass themselves off as the patient. In fact, this leads to medical identity theft – fraudsters buy stolen medical records from the black market and have all the information to pose successfully as the victim.
One other policy is to use patient ID wristbands. While this is a tad more secure than asking questions, it can still be taken off a patient and used for fraudulent purposes. Moreover, it is a contact-based solution, and that’s not something hospitals would want after the COVID-19 crisis – everyone is extremely aware of infection control issues now.
The most secure solution is using an identification policy where the identifier cannot be transferred or stolen – biometric modalities come to mind. There is a caveat though – patients would be quite reluctant to accept touch-based solutions such as fingerprint or palm-vein scanning.
Implement a touchless patient identification policy
The best option has been left for last – touchless patient identification platforms. RightPatient is the leading photo-based biometric patient identification system used by progressive healthcare providers.
Locking the medical records of patients with their photos upon registration, returning patients only need to look at the camera and the platform matches the photo with the one saved alongside their medical record, ensuring accurate patient identity verification.
There are many patient identification platforms available – be the responsible leader by choosing the one that shares the common goal of improving patient safety and quality of care at your facility.










 While COVID-19 and its long-lasting effects are raging on, that has not stopped hackers from attempting to steal sensitive patient data through healthcare data breaches. Security experts
While COVID-19 and its long-lasting effects are raging on, that has not stopped hackers from attempting to steal sensitive patient data through healthcare data breaches. Security experts