Healthcare Revenue Cycle Management Optimization is Crucial as In-Person Visits Increase

Believe it or not, while COVID-19 was arguably one of the worst problems faced by the U.S. healthcare system, it was just ONE of many. That’s right, there are a plethora of issues that have been hampering healthcare for years, causing patient safety incidents, lost revenue, and more. Unfortunately, these losses went through the roof due to COVID-19 – they were estimated to be around $323 billion in 2020. While the pandemic is slowly waning, things are going in the right direction as providers are opening their doors for in-person visits. To recover from the pandemic’s financial losses, healthcare revenue cycle management optimization must be one of the topmost priorities for health systems – let’s take a closer look at why it’s important and some strategies that can help with revenue cycle optimization.
Revenue cycle management in healthcare facilities
Healthcare revenue cycle management might be quite complex, as it contains many intricate processes, but it is simple enough to understand.
Revenue cycle management, in a nutshell, is used by hospitals and health systems to keep track of the “revenue” they receive by treating patients. It has many steps, but RCM starts from the first interaction with the patient, for instance, appointment scheduling, and continues until caregivers receive the final payment.
If broken down, revenue cycle of healthcare facilities usually contains 7 components:
- Preregistration
- Registration
- Charge capture
- Claim submission
- Remittance processing
- Insurance followup
- Patient collections
As this list shows, the revenue cycle starts from the first interaction with the patient and ends with receiving the full amount for providing healthcare services to the patient.
While it might seem simple, healthcare revenue cycle management is quite complicated and difficult, especially when it comes to collecting claims from the payers (insurance providers).
Why optimizing RCM has never been more crucial
While it was always important for healthcare providers to improve RCM within their facilities, doing so now might ensure their survival and get them through this trying time. COVID-19 has drastically affected healthcare providers, and while some received bailouts in billions, others had to close their doors permanently. The rest of them are simply struggling through the financial losses, but as in-person visits are increasing, things look brighter for the caregivers, as long as they are implementing strategies that optimize RCM right from the start.
That being said, let’s take a look at some of the strategies that can be employed to optimize healthcare revenue cycle management.
Strategies that enhance healthcare revenue cycle management
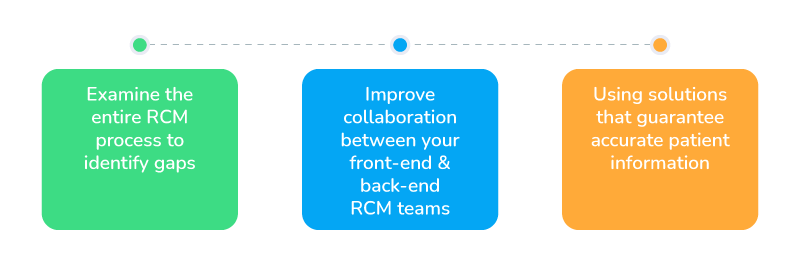
Examine the entire RCM process to identify gaps
While the age-old saying is “If it isn’t broke, don’t fix it”, rapidly evolving environments beg to differ. How do you know that it’s working out fine for you? Unless your denied claims are reduced to virtually zero, there’s always room for improvement.
Analyze the entire RCM process to see if there are addressable gaps that require improvement – even the smallest ones matter. Talk to patients, survey your RCM team, take a look at the current numbers, and determine where you want the numbers to be. If issues are not found, then great – the problem might not lie in RCM, but if issues exist, work on them. RCM is evolving rapidly, and with the changes brought about by COVID-19, introducing technology in almost every aspect of the service to improve efficiency and collaboration has become the new normal. And speaking of collaboration, let’s move to the next point.
Improve collaboration between your front-end and back-end RCM teams
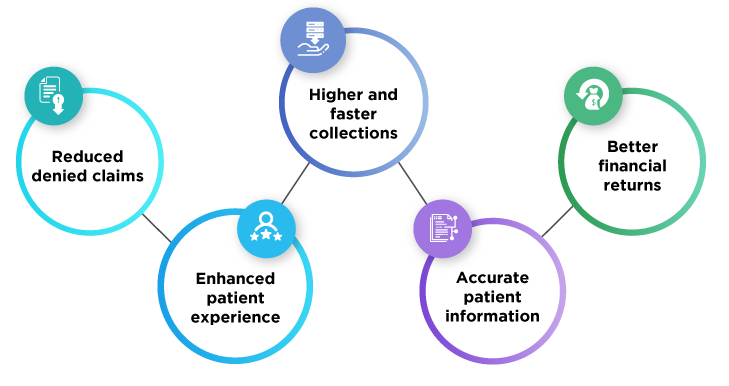
The traditional practice is that the front-end and back-end teams work towards the same goals, but separately. However, if they work more collaboratively then the entire process will become seamless and it will help optimize RCM as information is never lost or misinterpreted – helping to receive payments much faster and in greater numbers, improving the bottom line.
Using solutions that guarantee accurate patient information
When it comes to RCM, one of the biggest impediments to its optimization is denied or rejected claims – most of which can be traced back to billing and coding errors. On the front-end, if the patients are misidentified or if inaccurate medical records are used, then there are bound to be inconsistencies that are picked up by the payers. These errors lead not only to billing errors and denied claims, but can also be detrimental to positive patient outcomes – affecting the bottom line and the goodwill towards the hospital. As a result, ensuring patient data integrity and accurate patient identification is a must – both of which can be done with RightPatient.
RightPatient is a tried and tested biometric patient ID platform that safely and accurately identifies patients using their faces. The patient only needs to look at the camera – the platform does the rest, making it an entirely contactless process, something that is crucial in the post-pandemic world.
Not only does RightPatient make identification faster and accurate, but it also ensures that accurate information is fed to the registered patients’ EHRs every time they opt for healthcare visits, reducing billing and coding inconsistencies and denied claims in the process.