Hospitals Need a Better Patient Matching System to Identify “John Does”

Patient identification or lack thereof is a topic which we hear about every day. We always read news about mistaken patient identities due to mix-ups, frauds, insufficient patient matching system, etc. What about those who arrive at the hospitals and are never identified? Let’s look at these John Does but from a different angle – from the perspective of the emergency hospital staff who receive and treat them rather than from the outside viewer.

Imagine this: A man in his 50’s arrived in the emergency room, wheeled in by paramedics, shaven head, brown eyes, unconscious. To make matters worse, he had no materials on him that could have helped the staff with his identity for crosschecking with their patient matching system – no wallet, cellphone, papers, or anything at all. To top it all off, he did not have any distinguishing features such as a tattoo or scar. This incident was back in 2017 – a car hit him in January, and he was rushed in with a fatal brain injury to Los Angeles County+USC Medical Center. He did not have any visitors, nor was he ever reported missing. Sadly, he passed away being a John Doe, no one ever knowing who he was.
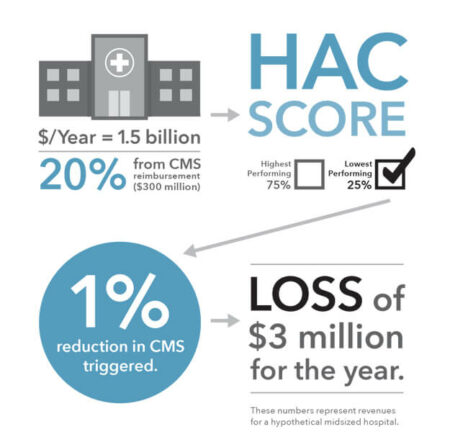
This is just one example of how serious and pressurizing it is for the hospital staff to deal with such emergencies regarding patient matching systems, primarily when they consist of a John Doe. In these cases, they are required to become a form of detective in order to determine the identities of these unknown patients when they arrive at the hospitals. This is done for several reasons: firstly, finding the identity helps with the treatment – the staff can then determine the patient’s medical history and whether he/she has any complications or not. Also, it allows them to find and contact a next of kin or close one to make any critical decisions if it becomes necessary. The identity also helps the hospital to contact the insurance company or government health programs, whichever the patient is associated with, regarding payment of their services.
However, there is a catch – federal laws concerning privacy make it difficult for the hospital staff to determine the unknown patients’ identities. In the previously mentioned example as well as in many similar cases, the team along with the social workers frantically rummage through whatever a John Doe brings with him – bag, clothing, phones without passwords, receipts, or whatever piece of document or device which can help them identify the individual and proceed to their patient matching system. Their efforts don’t stop there – they also question the paramedics and dispatchers. Tattoos, piercings, and scars are duly noted, and when all else fails, dental records are checked against the individual. However, because the police can only access fingerprints, it is often left unchecked, mainly because the police only involve themselves only when a criminal element is present in the situation.
These John Does are usually the ones hit by vehicles and had unfortunately left their IDs back at home, and can also be poor people with cognitive diseases such as Alzheimer’s. Other times, they are overdosed individuals. Unsurprisingly, socially isolated individuals like homeless people are the ones who are the most difficult to identify, and sadly, they are the ones who are the most common John Does in recent years.
The Health Insurance Portability and Accountability Act (HIPAA) was made to ensure the privacy of an individual’s medical data. However, in cases of these John Does, it can make patient matching increasingly difficult as the hospitals cannot release any information to those searching for missing family members regarding these patients. For instance, a patient with Alzheimer’s was admitted to a NY hospital with the name “Trauma XXX.” The police and his family members went in search for him several times at the very same hospital, but they were told nothing. Weeks later, a doctor while watching television saw that man in the news and identified him as the patient “Trauma XXX.” Afterward, when charged with why the hospital hid the patient, the staff said that they did not ask about “Trauma XXX” specifically.
Due to this incident, a lot of rules were set up and changed regarding information requests about missing persons. It consisted of following over twenty steps for hospitals, starting from notifying the reception, to taking DNA samples.
All of this could have been avoided if a fast, accurate, and reliable patient matching system was used. RightPatient is one such patient identification system that utilizes biometrics and AI. Through this, it uses iris scanning to quickly match the patients with their EHRs so that the whole patient experience can be enhanced. It also helps the physicians focus on more critical tasks such as the patients themselves instead of going through matching patients. Thus, not only is it beneficial for the patients, but it is also beneficial for the hospitals as well, creating a win-win situation for all and ensuring patient safety through the enhancement of the whole patient experience.