Leveraging Biometrics for Enhanced Data Security in Digital Healthcare

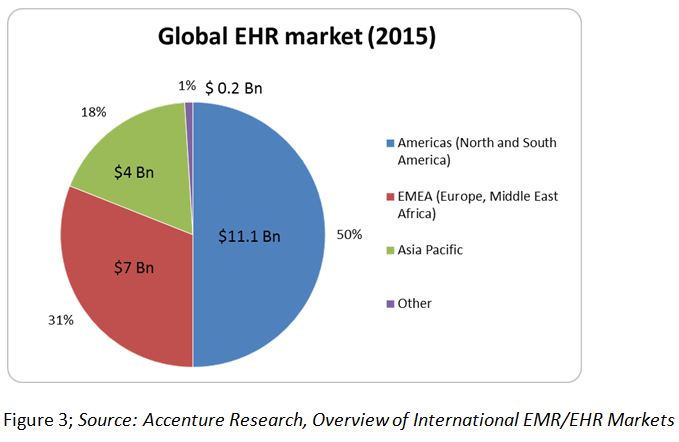
In the digital era, healthcare systems worldwide are actively embracing the power of technology to revolutionize the way they deliver care. However, this digital transformation is not without its challenges. Among these, the heightened risk of data breaches and identity theft is causing significant concern. According to recent projections, the cost of healthcare data breaches is estimated to reach a staggering $4 billion by 2020. This startling statistic underscores the urgent need for robust data security measures in the healthcare sector. RightPatient, a leading biometric patient identification solution, is at the forefront of addressing this critical need.
The RightPatient solution leverages advanced biometric technology to provide secure access to Protected Health Information (PHI), significantly mitigating the risk of data breaches and identity theft. Its state-of-the-art identification system ensures that only the right individuals have access to sensitive health information, thus preventing unauthorized access and ensuring the privacy and security of the patients’ data.
But the effectiveness of RightPatient extends beyond data security. The solution also plays a crucial role in enhancing patient engagement. By providing secure access to their PHI, RightPatient empowers patients to be more actively involved in their healthcare journey. This fosters a collaborative environment conducive to better patient outcomes and propels patients to take ownership of their health.
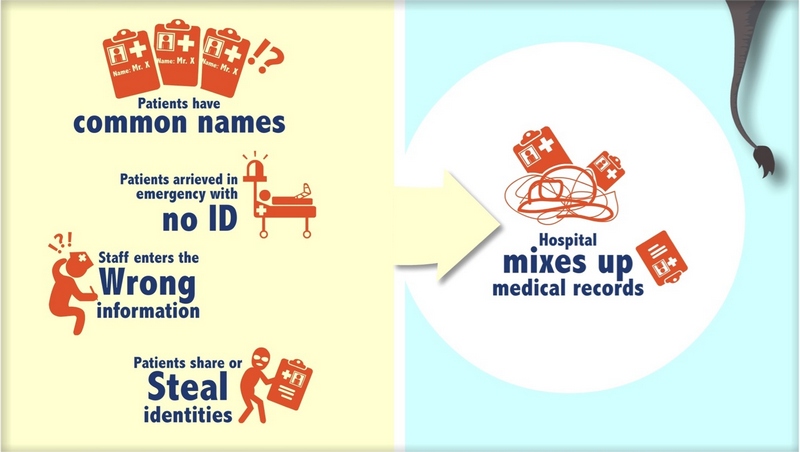
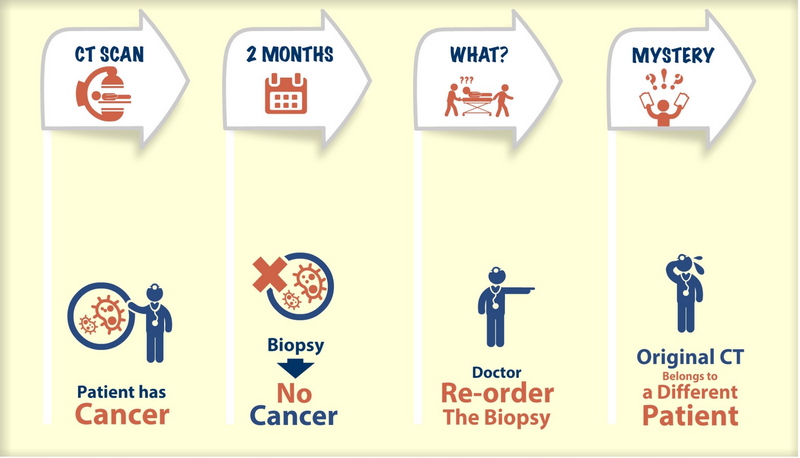
The value of RightPatient was significantly demonstrated when it was integrated into the healthcare system of International Health Management, a reputable NGO in Bangladesh. The organization was grappling with challenges such as incorrect patient identification, leading to issues like duplicate records, errors in medication distribution, and fraud. The introduction of RightPatient’s secure and efficient fingerprint biometric identification system in 2014 effectively eradicated these problems, benefiting about 5,000 patients across five distinct locations in the country. This real-world application underlines the potential of RightPatient in boosting data security and patient engagement in the digital health realm.
As we look to the future of digital health, the importance of biometrics cannot be overstated. RightPatient is more than just a solution to today’s digital challenges in healthcare; it’s a future-ready platform equipped to handle upcoming trends and innovations. It offers a smooth, safe, and hygienic way for patients to connect with their healthcare providers, positioning it at the forefront of digital health trends and innovations.
Experience the RightPatient difference in securing your digital health landscape – schedule a demo today. It’s time to embrace the digital health movement with the confidence of biometric technology. With RightPatient, healthcare providers can confidently integrate digital systems into their care delivery without compromising safety or privacy. Experience the power of biometrics, and secure your healthcare data with RightPatient.
How to Secure Your Healthcare Data with RightPatient
- Understand the Importance of Biometrics: Read our blog post on the importance of biometrics to understand how biometric technology can revolutionize healthcare data security.
- Explore the RightPatient Solution: Learn about the leading biometric patient identification solution and how it leverages advanced biometric technology to secure PHI.
- Schedule a Demo: Experience the RightPatient difference by scheduling a demo. This will give you a firsthand experience of how RightPatient can secure your healthcare data and enhance patient engagement.
FAQs
- What is RightPatient?
RightPatient is a touchless biometric patient identification solution designed to enhance data security and patient engagement in the digital health landscape. - How does RightPatient enhance data security?
RightPatient employs advanced biometric technology to provide secure access to Protected Health Information (PHI), significantly reducing the risk of data breaches and medical identity theft. - How does RightPatient foster patient engagement?
By providing secure access to their PHI, RightPatient empowers patients to take an active role in their healthcare journey, fostering a collaborative healthcare environment. - What makes RightPatient a future-ready platform?
RightPatient is equipped to handle upcoming trends and innovations in the digital health realm. It offers a seamless, safe, and hygienic way for patients to connect with their healthcare providers, positioning it at the forefront of digital health trends and innovations. - How can I experience the RightPatient difference?
You can schedule a demo to experience the RightPatient difference in securing your digital health landscape.














 Brad Marshall is a Senior Enterprise Development Consultant with RightPatient® With several years of experience implementing both large and small scale biometric patient identification projects in healthcare, Brad works closely with key hospital executives and front line staff to ensure project success.
Brad Marshall is a Senior Enterprise Development Consultant with RightPatient® With several years of experience implementing both large and small scale biometric patient identification projects in healthcare, Brad works closely with key hospital executives and front line staff to ensure project success.











