Improving Healthcare Safety with Accurate Patient Identification

Can you imagine, almost 10% of patients are wrongly identified during medical record verifications? This staggering statistic emphasizes the critical importance of patient identification in healthcare. In this piece, we delve into the profound connection between patient safety and patient identification, highlighting the potential risks and repercussions of imprecise patient identification and its impact on healthcare interoperability and data precision.
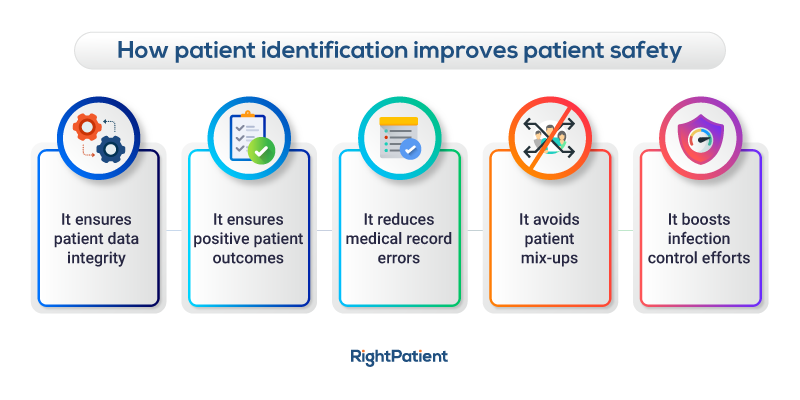
Patient misidentification can lead to severe hazards, including compromised data precision and interoperability issues. Such mistakes can have a direct bearing on patient safety, resulting in medication inaccuracies, unnecessary surgeries, and incorrect patient data. In such a complex, high-risk environment, precise patient identification is not merely desirable. It is a life-saving measure.
Welcome to RightPatient, an innovative patient identification solution that transforms patient safety. Leveraging cutting-edge technology, RightPatient guarantees the correct identification of patients, enhancing the safety and effectiveness of healthcare services. It acts as a digital shield, a primary defensive line against the pitfalls of erroneous patient identity.
Consider the example of International Health Management, a prestigious NGO delivering high-quality healthcare services in various urban and rural areas of Bangladesh. They grappled with inaccurate patient identification, causing a range of issues like duplicate patient records and medication distribution errors. In their pursuit of a solution, they incorporated RightPatient’s web-based fingerprint biometric identification system into their healthcare framework. The outcome was smooth, accurate, and speedy patient identification.
Utilizing unique biometric modalities like fingerprints, RightPatient ensures accurate patient identification in seconds. It not only prevents the creation of duplicate medical records and medication errors but significantly minimizes the potential risks and repercussions of medical fraud and identity theft. This reinstates the confidence of patients in healthcare services.
RightPatient does more than just improve patient safety – it also fortifies financial health by mitigating costs linked to misidentification. With RightPatient, healthcare providers embark on a path towards enhanced patient safety, improved data integrity, and interoperability. Enjoy the tranquility that comes with the assurance that your patients are accurately identified, every single time.
Step into a new era of patient safety with RightPatient, where healthcare, technology, and trust converge into a harmonious symphony of wellbeing. To discover more about how RightPatient can revolutionize your healthcare services, visit our website or get in touch with us directly.
How to Use RightPatient
- Choose RightPatient: Commit to consistent, reliable patient identification for improved data integrity, interoperability, and patient safety. Visit our website to get started.
- Implement RightPatient: Incorporate RightPatient's web-based fingerprint biometric identification system into your healthcare framework. Learn more about our biometric patient identification solution.
- Experience the Benefits: Enjoy the tranquility that comes with the assurance that your patients are accurately identified, every single time. Discover how RightPatient can fortify your financial health by mitigating costs linked to misidentification.
FAQs
- What is RightPatient?
RightPatient is an innovative patient identification solution that ensures accurate identification of patients, enhancing the safety and effectiveness of healthcare services. - How does RightPatient improve patient safety?
RightPatient mitigates the risks of patient misidentification, which can lead to severe hazards like medication inaccuracies, unnecessary surgeries, and incorrect patient data. It acts as a digital shield against these pitfalls. - What technology does RightPatient use for patient identification?
RightPatient utilizes unique biometric modalities like fingerprints for accurate patient identification. - Does RightPatient only improve patient safety?
No, RightPatient also fortifies financial health by mitigating costs linked to misidentification, improving data integrity and interoperability. - How does RightPatient prevent the creation of duplicate medical records?
By ensuring accurate patient identification, RightPatient prevents the creation of duplicate medical records, which can lead to medication errors and other potential risks.