How to Improve Healthcare Outcomes and Reduce Readmission Rates

Improving a patient’s outcome (for instance, their quality of life or life expectancy) is obviously the prime reason for treating them. Patients approach a medical professional with the hope of ‘being cured’ of whatever ails them, whether that’s by being prescribed medication to ease symptoms or having an operation or procedure to relieve pain or remove or transplant a body part to offer a better quality of life. When they are paying for their treatment, they have every right to expect that their life is better afterward. Hospitals that do not achieve the required levels of treatment outcome are routinely penalized, thus, they need to improve healthcare outcomes. These levels are measured by readmission rates. On average, over 2,500 hospitals are likely to be penalized because of their monthly readmission rates, even though the pandemic will have increased the chances of some patients having to be readmitted.

Improve healthcare outcomes with an effective patient identification platform
However, there are some very simple ways in which hospitals can improve healthcare outcomes and reduce readmission rates.
Identify your patient. Continue to identify your patient.
Correct patient identification is key. Ensuring that staff members are treating the right patient for the right ailment is, perhaps, needless to say, the best way to improve healthcare outcomes. Getting identification wrong can lead to any number of issues, from unnecessary operations or incorrect scans to potentially dangerous prescription medication being offered.
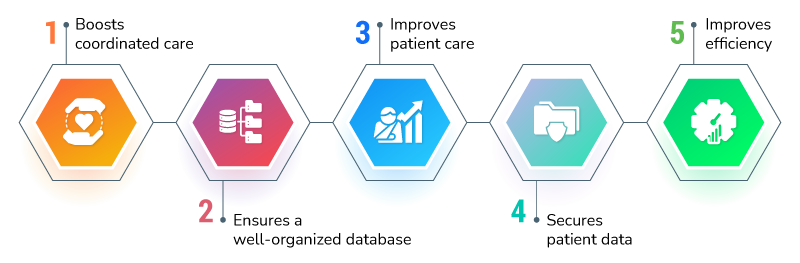
The best way of ensuring correct patient identification is by using a touchless biometric patient identification platform such as RightPatient. It helps improve healthcare outcomes, ensures timely sharing of appropriate information with other professionals, and ultimately helps lower the chances of a patient safety incident.
The data may be on the screen, and may well be correct. But front desk staff, nurses, medics, and others are only going to know this for sure if they use such a solution. The available data is also likely to show previous admissions, incidents that the patient may have been involved in, allergies, vital statistics, next of kin, and areas of concern for the patient’s health.
Many hospitals undertake patient surveys to help them improve patient care, and this option can be offered as a patient reaches discharge date, if appropriate.
Goals, KPIs, outcomes, HSMRs – whatever you call them, they help improve healthcare outcomes.
Improving the patient’s experience of their stay in the hospital will also improve their view of how well they were treated. A positive outlook has been shown to raise recovery rates. Plus, helping patients recover makes staff feel better too. Making a good outcome a key goal of the organization and the staff will help both sides. Suggesting a reduction in incidents from the previous year is a friendly way to ask for an improvement in figures, whilst still recognizing that employees are human and can make mistakes.

RightPatient identifies patient records accurately
No matter how good the records, unnecessary scans can be requested and patient information can be incorrectly recorded. It happens. If the patient’s identity can be verified accurately, then mistakes can be avoided.
Sharing is caring.
Sharing information with other caregivers can also improve healthcare outcomes and provide healthcare professionals with a rounded picture of the person they are treating. Not all patients will be happy with this option, but for primary care doctors, knowing where else their patients have already been treated is of great benefit when referring them to other specialties. Many people have to see a different physician for every ailment, and joined up care can make things much easier. When someone with a chronic condition ends up in the ER, a shared electronic health record allows everyone to know what medication the patient has already been prescribed and even whether certain common treatments have already been attempted.
CMS, therefore, requires healthcare providers to use CoP electronic notifications to let other named physicians know that they have a patient in their care. These notifications also alert others in the chain about patient discharge or transfer, which is important for ongoing care – using RightPatient can help with that. RightPatient also aims to prevent duplicate medical records, so acting against medical identity theft. All of this helps CMS compliance, which is good news for a facility’s finances, as fines for CMS breaches can be crippling after a while.
Contact us for more information on how RightPatient can help your facility and your patients stay safer from medical mix-ups and online impersonation by using our biometric patient identity management system.