Value-Based Care: A Patient-Centered Approach Requires Knowing Your Patient

Aspirin, penicillin, monoclonal antibodies, interventional cardiology, and genome editing have undoubtedly revolutionized medicine. However, while all of these have been breakthroughs in the field of medicine, not much has changed in the way that doctors do their jobs. Patients visit their doctors, the doctors diagnose, they recommend tests, they prescribe drugs, and they are compensated according to the volume of work done or the number of procedures performed.

If medicine is to progress in the 21st century, things have to change at every level, including the way that doctors work and receive compensation, the way they identify the right patient, and the way that patients are treated.
The long-awaited system that is going to change the way doctors work and are compensated will soon become a reality. This new system is called value-based care.
Value-based care is about compensating doctors according to outcomes. This encourages more personal attention to patients and transitions the healthcare system from cure-based to preventive medicine. It is a system in which doctors receive a higher level of compensation for either better outcomes from procedures or enabling patients to avoid health-related problems altogether.
There are several benefits of a healthcare system where the right patient gets the right kind of care.
Value-based care can save patients a lot of money. Putting aside the historical projections of healthcare inflation, the U.S. is also facing major epidemics of chronic, non-communicative diseases like diabetes, high-blood pressure, and cancer. It is no secret that many of these ailments are preventable with timely intervention and/or the correct behavior. Value-based care creates an environment where doctors can help patients to avoid these diseases by intervening at the right time. A doctor would identify the right patient to design a prevention plan before a disease can manifest where things become more complicated and expensive.
Once the right patient, a patient with a high risk of developing a chronic illness, has been identified, the doctor would be encouraged to spend more time with her, teaching her to take better care of herself so that complications can be avoided. There would be a reward system for identifying the right patient and taking timely preventative measures. It would also result in higher patient satisfaction.
A value-based care system would also lower drug costs. Historically, manufacturers decide the price of their medications without taking into consideration the value that a particular drug has in terms of its effectiveness and overall patient wellbeing. A value-based system would also encourage the development of personalized medicine where treatment plans and even pharmaceuticals can be tailored to specific patient needs.
The backbone of the value-based care system would be patient identification and data mining. Many are already demonstrating why medicine should incorporate more data-based modeling to augment physician decision-making. Data mining helps doctors and the healthcare industry as a whole to better understand the outcomes of various therapeutic approaches. Ultimately, it can help to create the right kind of individualized solution for the right patient.
Unfortunately, realizing optimal results from data mining and value-based care has its challenges, especially as healthcare organizations start mining data that has been accumulated over long periods of time. On average, at least 8% of hospital patient records consist of duplicate data. Thus, an intelligent way to sort out these duplications and identify the right patient is desperately needed.
It is stated that value-based care is about the right patient getting the “right care, in the right place and at the right time.” Instead, the maxim should be, “RightPatient® enables the right care, in the right place, at the right time.”
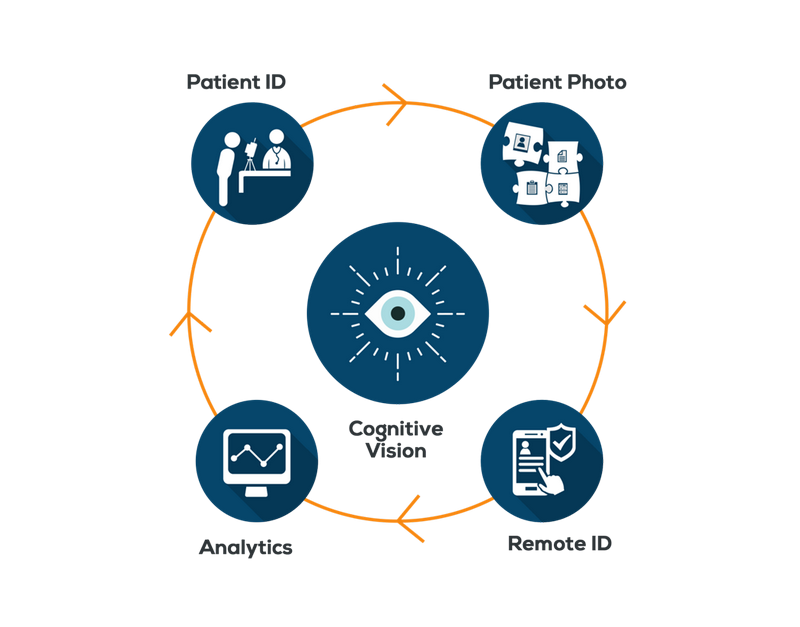
RightPatient® guarantees that a patient medical record is never mixed up with another record and the hospital ecosystem will always recognize the patient with the help of cognitive vision. Mistakes from common patient names, fraud, human error and other issues are always prevented.
As we all know, chains are only as strong as their weakest link. In many hospitals or medical institutions, there is an urgent need to strengthen this weakest link throughout the entire system – overcoming the errors of false identity and data duplication with RightPatient. Only then can the benefits of value-based care and data mining be fully realized.