Electronic Medical Record Errors Are Preventable with Positive Patient Identification

We’ve been talking about several topics such as medical identity theft, duplicate medical records, COVID-19, revenue cycle management, data breaches, and more. However, the one point we keep coming back to is electronic medical record errors. This has been a cause of concern among healthcare providers and patients, but it doesn’t end there. The consequences of medical record errors extend to insurance providers, healthcare staff members, physicians, and even the patients’ family members!
What many fail to grasp is that most of these errors are not caused by the EHR systems themselves, but are caused by external factors. One of the foremost reasons is that there’s no effective, standardized patient identifier present. This alone leads to medical record mix-ups, duplicates, and other errors – more on that later.
Let’s take a look at EHR error statistics, the consequences caused by them, and how positive patient identification can mitigate them.
Statistics regarding electronic medical record errors
A recent study focused on the frequency and types of EHR issues perceived by patients which shed light on a number of insightful statistics. Over 136,000 patients received the invitation to participate, and over 29,000 patients responded. 22,889 viewed 1 or more notes within one year. Out of these 22,889 patients, 21% (4,830) of them witnessed mistakes. Out of these 4,830 patients, 43% said that the mistakes were serious, 32.4% said that it was somewhat serious, and 9.9% said that it was very serious.
When asked about what kind of issues they saw within their EHRs, the most common response was diagnosis errors. For instance, many saw that a disease they didn’t have was listed in the EHR! Can you imagine the consequences of this?
Others witnessed wrong medical history, medication errors, and so on.
Most of these issues, if not all of them, can be traced back to the lack of accurate patient identification – let’s see how.
How patient misidentification creates electronic medical record errors
It’s quite simple – since there’s no effective and standardized patient identifier present in the U.S. healthcare system, EHR issues are bound to occur. An EHR system houses thousands and can even hold millions of medical records. It’s quite natural to have many patients with the same name, especially if it’s a common one.
Now, if a patient named “James Smith” turns up, the EHR user will see that there are several medical records associated with the same name. Moreover, there’s no guarantee that the patient’s record is under the same name – it might be saved as “Jim Smith”.
Also, most EHRs provide basic search functionality, and with the registration area being a high-pressure environment, the EHR user needs to select the appropriate medical record quickly. If the hospital isn’t using an effective patient identifier, the registrar either creates an entirely new medical record or chooses the wrong one – creating the potential for medical record errors.
While that’s how patient misidentification and electronic medical record errors are related, let’s take a look at some of the consequences.
Consequences of EHR errors and patient misidentification
EHR errors, bolstered by inaccurate patient identification:
- Increase duplicates and overlays within the EHR system
- Jeopardize patient safety
- Hamper patient data integrity
- Lead to patient record mix-ups
- Create medication administration errors
- Increase denied claims
- Cause patients to go through repeated lab tests
- Increase hospital readmissions
- Create detrimental patient outcomes
It’s not very surprising that patient identification errors have been occurring for a long time, and only a handful of healthcare providers have been proactive regarding preventing such issues within their facilities. These responsible healthcare providers have been using RightPatient to prevent such issues by ensuring accurate patient identification.
RightPatient ensures positive patient identification
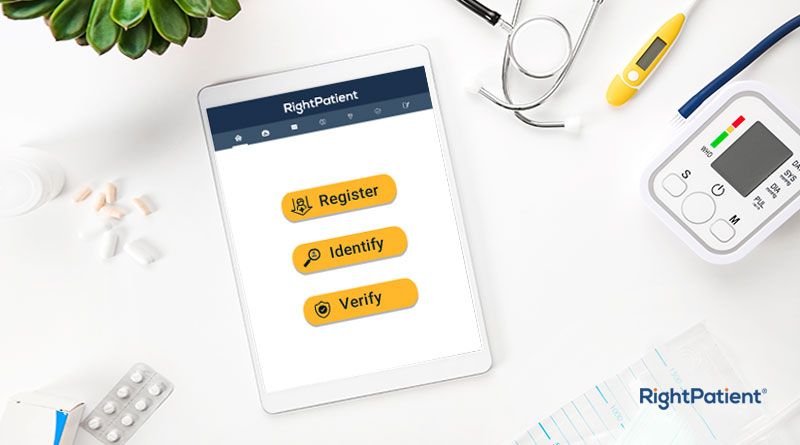
RightPatient is the number one choice of leading healthcare providers – they’ve been using our touchless biometric patient identification platform to protect millions of patient records.
RightPatient is easy to use and becomes a part of the EHR workflow. During registration, the platform requires patients to simply look at the camera – the platform takes a photo of the patient and essentially “locks” the EHR with it. Already registered patients then only need to look at the camera – RightPatient runs a search to match the live photo with the saved one – it’s that easy!
RightPatient has a vast amount of experience with several diverse hospitals, making it a clear choice to ensure accurate patient identification, prevent medical record errors, and more.
Are YOU preventing medical record errors successfully at your healthcare facility?