5 Ways EHR benefits Healthcare Providers and Patients

Usually, our blog mostly talks about the issues that plague the US healthcare system. Moreover, the majority of 2020 did not give much scope to talk about anything positive, especially in the healthcare space. It has been a rollercoaster ride for all of us, and with the breakthrough vaccines, all of that is hopefully behind us. That being said, we wanted to focus on something positive this time around – the benefits of EHR (electronic health record) systems. They have been in use for years and most of us have taken them for granted. However, EHR systems provide a host of benefits for everyone involved – making processes more streamlined, boosting coordinated care, and improving patient care. Let’s take a look at 5 ways EHR benefits both healthcare providers and patients and how it improves healthcare outcomes.

5 ways in which EHR benefits healthcare
Before electronic health records, healthcare providers used paper records. While they had some benefits at the time, they had a number of drawbacks as well. For instance, paper medical records took up a significant amount of space. If a hospital has thousands of patients, where would all the records be stored? Moreover using paper was not feasible – if you made mistakes, then they had to be crossed out and rewritten. Finally, it was extremely difficult to search for paper medical records. All of these issues are eliminated with electronic health records.
While the aforementioned were some commonly known EHR benefits, let’s take a look at how it improves healthcare.
Boosts coordinated care
In the earlier decades, patients usually had visited a single hospital, had a single healthcare provider, and all of their doctors were from the same system. Now, healthcare has become complex, includes physicians from different hospitals, and requires all of them to communicate to provide better and coordinated care.
EHR benefits coordinated care efforts significantly. The physicians of a single patient can access their digital medical records that are kept at a centralized location. They can make necessary changes, obtain critical information, and make informed decisions, all of which are recorded within the EHRs, helping everyone to work together.
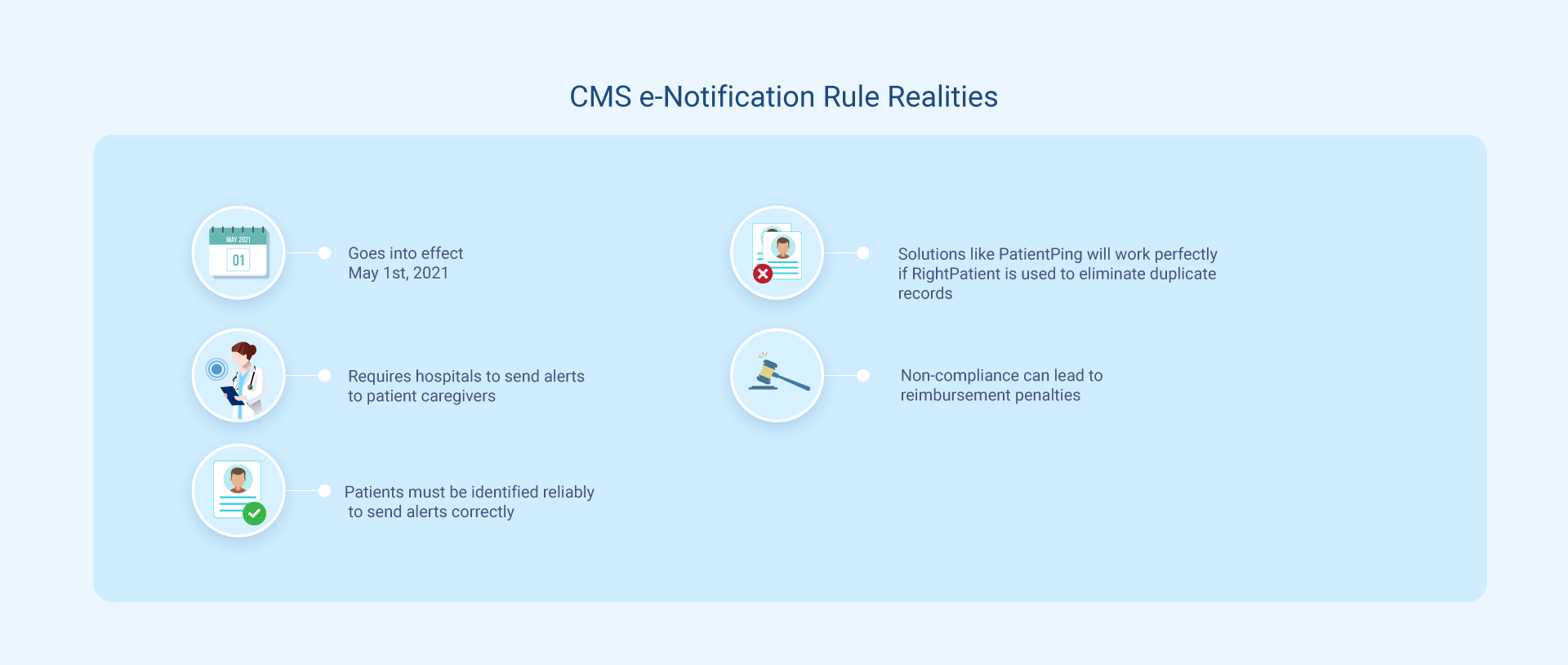
CMS has also mandated healthcare providers using EHR systems to support e-notifications in order to boost interoperability and enhance coordinated care. Fortunately, RightPatient can help send out accurate alerts and prevent false ones.
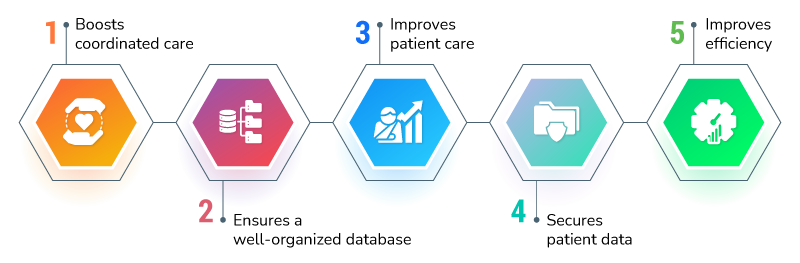
Ensures a well-organized database
Since EHRs are digital, they need to be stored somewhere – a database, to be precise. With EHR systems, healthcare providers can store their data in a centralized location if they choose to do so, as many of them back up the data in other locations. As all of the data is in a single location, it is much easier to manage, access, update, and keep track of activities such as changes made.
EHR benefits patient care
Interrelated with the previous points, EHRs help enhance patient care, as information is retrieved and stored faster, something that is critical during time-sensitive cases to make informed decisions. Moreover, most of these records are virtually error-free, and if not, they can be rectified whenever required.
Secures patient data
EHRs don’t have the risks associated with paper records – fire, water, or some other damage won’t be able to affect them. Moreover, most healthcare providers keep backups, so, in cases of emergency, the backups can be used. Moreover, the information is encrypted and sent via secure means, rendering it useless for hackers in most cases.
Improves efficiency
As previously mentioned, EHR systems dramatically improve efficiency. Prior to EHRs, caregivers had to search for the record manually and send faxed copies to labs, or other caregivers – something which was not secure, and recordkeeping was quite problematic. For instance, imagine that you sent a record of 4 pages, but you got back 10 pages in return that contained new information – recordkeeping was an administrative nightmare!

With EHRs, the healthcare staff member simply puts the name in the search bar, identifies the accurate medical record, and sends it over securely. The EHR user doesn’t need to accommodate the new information; it automatically gets recorded in the original record, making everything more efficient than ever. Also, healthcare teams don’t need to visit each other to send over the records – one click and it’s sent over to the required individuals, saving time and costs.
RightPatient boosts EHR benefits
While EHRs have a number of advantages it brings for healthcare providers and patients, some external factors hinder them from providing the best possible experience. One such restriction is patient identification.
The unique patient identifier (UPI) was supposed to be made around two decades ago, but due to privacy concerns, a ban was imposed on its funding. As a result, healthcare providers still struggle with patient identification errors. Not everyone faces these issues, though, many use RightPatient.
RightPatient is a touchless biometric patient identification platform used by several responsible healthcare providers and clinics. It identifies patients accurately across the care continuum and becomes part of the EHR workflow.
During enrollment, patients only need to look at the camera – the platform captures a photo and their biometric data and attaches them to their EHRs. Returning patients just have to look at the camera – RightPatient runs a search and provides accurate medical records in seconds, boosting EHR efficiency. The best part is that the process is entirely touchless, eliminating any chances for HAIs (hospital-acquired infections), making it ideal to be used in the post-pandemic world.
RightPatient also prevents duplicate medical records and overlays – something that is extremely crucial to improve healthcare operations.
RightPatient enhances patient safety, improves patient outcomes, prevents medical identity theft, and boosts the bottom lines of healthcare providers – something that is vital right now to survive during the pandemic. Be a responsible healthcare provider and contact us now to learn how we can help your healthcare facility.