Leveraging Multi-Modal Biometric Identification for Enhanced Patient Care

The healthcare sector is continually evolving, and the advent of innovative technologies has been reshaping patient identification processes, enhancing data integrity, and improving overall patient care. This transformation is driving a shift from single modality identification systems to a more comprehensive and effective multi-modal biometric identification system like the RightPatient® system. Such a system can accurately identify patients across various touchpoints, from bedside healthcare services to home health, emergency rooms, or mobile environments. It’s not just a vision of the future; it’s a reality that is being progressively shaped by technological advancements and the pressing need for accurate patient identification.
These systems, relying on a single form of patient identification, such as fingerprints or iris scans, have struggled to adapt to the rapidly changing healthcare environment. This inability to keep pace has led to a multitude of problems, including patient misidentification, duplicate records, and issues related to medical identity theft.
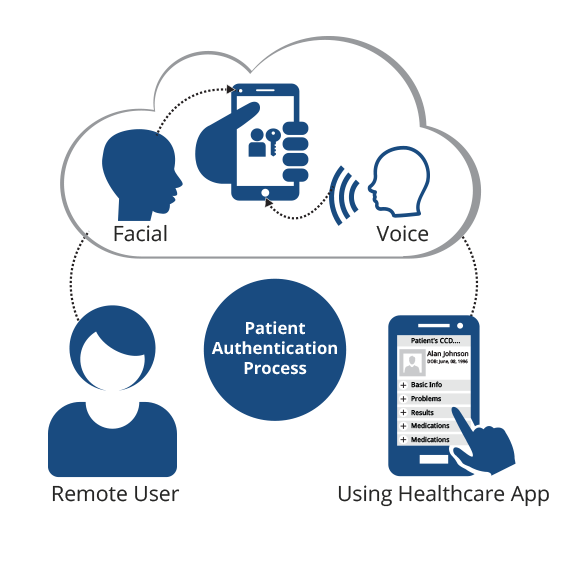
Multi-modal biometric identification systems like RightPatient®, on the other hand, harness the power of cutting-edge voice and facial recognition technologies. They offer a robust solution to the issues plaguing single modality systems. RightPatient®’s extensive capabilities to authenticate patient identities across various touchpoints make it a beacon of hope in an increasingly complex healthcare landscape.
A practical example of the effectiveness of the RightPatient® system is seen in the case of International Health Management, a well-respected NGO that runs healthcare projects in Bangladesh. After dealing with numerous issues related to incorrect patient identification, the organization integrated RightPatient® into their healthcare framework. The results were dramatic, with the system accurately identifying approximately 5,000 patients across five different locations within the country. This example not only showcases the effectiveness of RightPatient® in improving patient identification but also highlights its adaptability to different patient touchpoints, demonstrating the system’s flexibility, scalability, and integrity.
RightPatient® is not just a solution for the present; it’s future-ready, compatible with any biometric form, including fingerprint, finger vein, palm vein, iris, facial, and voice recognition. This broad compatibility makes it an ideal choice for institutions planning to evolve their patient identification touchpoints in the future.
In conclusion, as healthcare touchpoints continue to diversify, the need for multi-modal biometric identification systems like RightPatient® becomes increasingly evident. They offer more than just functionality — they guarantee the highest levels of patient engagement, safety, and long-term value. These systems are not just the future of patient identification; they’re the present, reshaping the healthcare industry and ensuring improved patient care and data integrity. For more information about RightPatient®, visit https://www.rightpatient.com/ or contact us at https://www.rightpatient.com/contact/.
How To
- How to Integrate RightPatient® into Your Healthcare Framework
RightPatient® integrates seamlessly with the healthcare workflow. For a smooth setup process, follow the instructions provided by our team. For more insights, check out our blog post on Why We Offer a Choice of Hardware Modalities for Biometric Patient ID. - How to Leverage RightPatient® for Accurate Patient Identification
RightPatient® uses voice and facial recognition technologies for patient identification. Learn more about these technologies in our blog post on Improving Mobile Patient Identification with Wireless Technology. - How to Future-Proof Your Patient Identification Process with RightPatient®
RightPatient® is compatible with any biometric form, making it a future-proof solution. Read our blog post on Why Experience Matters When Selecting a Biometric Patient Identification Solution to understand how to make the most of this feature.
FAQs
- What is RightPatient®?
RightPatient® is a multi-modal biometric identification system designed to accurately identify patients across various healthcare touchpoints. - How does RightPatient® differ from single modality identification systems?
Unlike single modality systems that rely on one form of patient identification, RightPatient® leverages cutting-edge voice and facial recognition technologies to offer a robust solution to patient misidentification, duplicate records, and medical identity theft. - Is RightPatient® adaptable to different patient touchpoints?
Yes, RightPatient® has proven its adaptability across different patient touchpoints, including bedside healthcare services, home health, emergency rooms, and mobile environments. - Is RightPatient® future-ready?
Yes, RightPatient® is compatible with any biometric form, making it an ideal choice for institutions planning to evolve their patient identification touchpoints in the future. - Where can I get more information about RightPatient®?
For more information about RightPatient®, visit https://www.rightpatient.com/ or contact us at https://www.rightpatient.com/contact/.