Common Reasons for Patient Identification Errors in Hospitals and How to Solve Them

Positive patient identification is an important but underappreciated component of the US healthcare system. Healthcare providers maintain patient safety, appropriate medical treatment, and good healthcare results by precisely identifying patients and using their relevant electronic health information. For instance, the physicians know of the patient’s comprehensive medical history, the revenue cycle team knows which claims to submit to the insurer, and the hospital records the patient’s information in the appropriate EHR. Unfortunately, this isn’t always the case; patient identification errors in hospitals are all too common and can generate a slew of issues for healthcare providers, patients, and insurance companies.
Patient identification errors in hospitals generate a variety of issues, including:
- Patient safety issues
- Patient data integrity failure
- Patient mix-ups
- Medical record errors like duplicates and overlays
- Denied claims
- Detrimental patient experience
- Medication administration errors
- Financial and legal issues
While those are some of the issues created by patient misidentification, let’s look at some of the common reasons why they happen in the first place, as well as how a touchless biometric patient identification platform like RightPatient ensures positive patient identification.
Common reasons for patient identification errors in hospitals
Patient misidentification during registration
In hospitals, patient misidentification is most common during registration. Patients are wrongly identified and linked to the incorrect EHRs from the start during the registration procedure. As a result, the patient will receive ineffective care because the physicians will be relying on someone else’s medical history.
The patient’s EHR is difficult to find
The registration areas are arguably high-pressure situations, as patients are constantly arriving, and a limited number of workers are required to process them for treatment. However, when the registrar examines the EHR system, they may discover that no medical records match the patient. At times, registrars may detect that too many EHRs correspond to the patient. In these instances, registrars must select an EHR, and the chances are that they will select the erroneous one, resulting in improper patient identification.
Reducing patient waiting times
As previously said, any given healthcare provider’s registration area is quite hectic. Patients are begging for treatment, and registrars are under intense pressure to shorten patient wait times. Because there is no standardized precise patient identifier in place, searching for the relevant medical records can take a long time. Because the EHR system contains tens of thousands of medical records, the registrar may wind up picking the incorrect medical record.
Existing duplicate medical records
This may appear perplexing, but patient identification errors in hospitals and medical record errors are inextricably linked; the other will follow naturally if one occurs.
Patient identification, for example, occurs when an incorrect medical record is picked. When the registrar searches the EHR system and finds no EHRs with the patient’s name, they create a new medical record. However, due to a lack of definite patient identification, the patient’s genuine medical record could not be identified, resulting in a new duplicate medical record.
Similarly, duplicate medical records within the EHR system are bound to induce patient misidentification because all of the records are inconsistent and fragmented, resulting in patient safety issues, incorrect treatment, and worse.
Human errors
Human error is another prominent cause of patient misidentification in hospitals. While registrars, nurses, and other healthcare workers already work in a high-stress environment, a single typing error can force them to select the wrong EHR.
Patients themselves submit false, wrong, or incomplete
Patient misidentification in hospitals happens when patients offer insufficient or incorrect information to medical employees. For example, a patient’s medical record is maintained with the name “William Smith,” yet he gives the registrar the name “Bill Smith.” The registrar will search for his medical record using the keyword “Bill Smith,” which will not yield the genuine EHR.
On the other hand, patients falsify information to obtain treatment in the name of someone else. It’s nearly impossible to identify the falsehood because healthcare providers don’t employ a reliable patient identification system throughout the states.
RightPatient can prevent all of the above and more.
RightPatient prevents patient identification errors in hospitals
RightPatient is a touchless biometric patient identification platform that accurately identifies patients across the treatment continuum. During the registration process, the platform captures patients’ photographs and ties them to the proper EHRs, effectively locking the medical records. When the patients return, the platform must authenticate their identities – the patients only need to glance at the camera – it’s that simple!
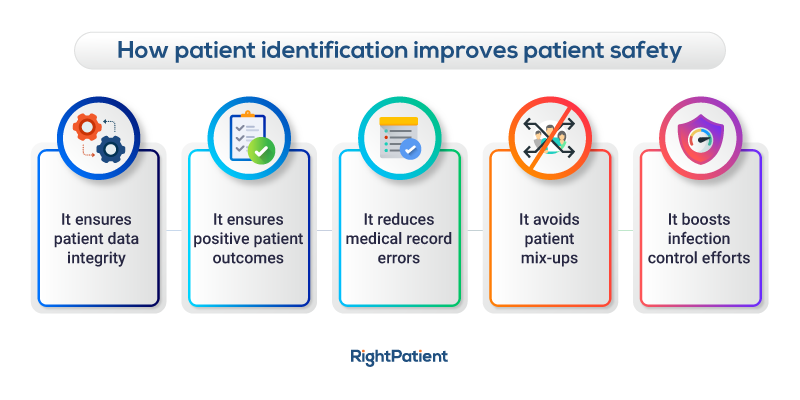
RightPatient enhances patient safety, minimizes denied claims, strengthens patient data integrity, and ensures that the proper patient is receiving the right treatment at all times.