6 Tips for Helping Your Patients Feel Safe in Your Office

The following guest post on patient safety in healthcare was submitted by Kara Masterson.
The relationship between patients and their medical care providers is fundamental to the effectiveness of treatment. A lot of people don’t feel comfortable in doctors’ offices, some more than others. Professionals such as dentists, counselors, and therapists can have a hard time dealing with scared patients. A doctor must have a way to forge a relationship and maintain it throughout, and that begins by making patients feel safe when they visit your office. Here are just a few tips to help make that possible:

Learn more about practical tips you can adopt at the doctor’s office to increase patient safety.
Polite Staff
Some of the fears that individuals have are results of bad experiences that start at the reception desk of a doctor’s office. The first encounter that a patient gets shapes their perception of how the place operates, so if it’s a bad one, it will affect how they behave when they see you. Ensure that all the staff members know how to talk to patients and keep the comfortable.
Non-Threatening Surroundings
Fear of a doctor’s office may arise from the environment that patients have to be in when they come for their appointments. This problem is, especially a common one in dentists’ offices where patients take one look and fear sets in. Bric-a-brac spread around the room can distract patients from intimidating tools or equipment present in the settings. Kid-friendly furniture, TV, toys, and play areas can also make your office more accommodating to kids.
Initiate Conversations
Some patients find it hard to open up when undergoing therapy, making it necessary to try a few tactics to get them to talk. Therapists and counselors who have been through social work doctoral programs have the skills to communicate with patients in ways that calm their fears. You should establish a technique to talk to patients that include using the right language, words, and tone.
Sensitivity
Good bedside manners will go a long way in getting rid of fears in your patients. Things like disrobing for tests can be uncomfortable for some people, so be sensitive to their feelings and reassure them when they need it. People always like having someone there for them that is sensitive to how they are feeling.
Explain
Doctors sometimes forget that patients don’t have an inherent knowledge of what they are talking about and ramble on and on when giving information. Take the time to lay out details for a patient and take them through every step. Don’t confuse patients with jargon. By taking time to explain to your patients in their language what is happening you can really help make them feel more comfortable.
Engage
A patient may have concerns such as the cost of treatment and financing options but may be too afraid to ask you upfront. The NCBH recommends engaging patients by asking questions to open opportunities.
Overall, there are tons of different things you can do to help your patients feel comfortable in your office. You want to make sure that you space is comfortable and secure for everyone that comes in it. Not only can that help make your patients feel good, but it can help you feel good as well.
Kara Masterson is a freelance writer from Utah. She graduated from the University of Utah and enjoys writing and spending time with her dog, Max.





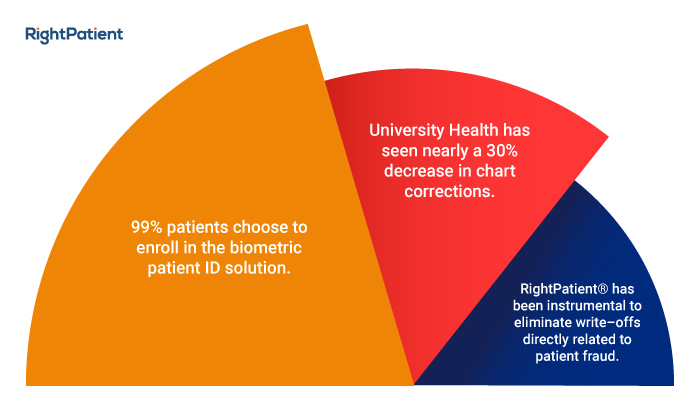
 Brad Marshall is an Enterprise Development Consultant with RightPatient®. With several years of experience implementing both large and small scale biometric patient identification projects in healthcare, Brad works closely with key hospital executives and front line staff to ensure project success.
Brad Marshall is an Enterprise Development Consultant with RightPatient®. With several years of experience implementing both large and small scale biometric patient identification projects in healthcare, Brad works closely with key hospital executives and front line staff to ensure project success.