Why Patient Photos Should Be Linked to Medical Records

The following post on why patient photos should be added to medical records to improve patient safety was submitted by Michael Trader, President and Co-Founder of RightPatient®
The Push to Increase Patient ID Accuracy and Safety
Achieving accurate patient identification in healthcare is an important catalyst to ensure safe, cost-effective care delivery. Although we believe that accurate patient ID should have received more attention and scrutiny parallel to the rapid digitization of the healthcare industry, the issue has finally been thrust into the spotlight by powerful organizations such as AHIMA, the ONC, and CHIME as something that must be solved in order for other mandates (e.g. interoperability, health information exchange, population health, etc.) to materialize.

Why aren’t more healthcare providers capturing patient photos during registration?
Many healthcare organizations have proactively addressed the lingering issue of accurate patient identification by implementing new technologies that supplement existing methods of obtaining demographic information, insurance cards, and proof of ID. The idea is to add biometrics as an added layer of identity protection, security, and identification accuracy by asking patients to provide a physiological token prior to accessing health data and/or medical services. Biometrics for patient ID has rapidly caught on as a proven method to prevent fraud and medical ID theft, improve data integrity, prevent duplicate medical records, and safeguard protected health information (PHI).
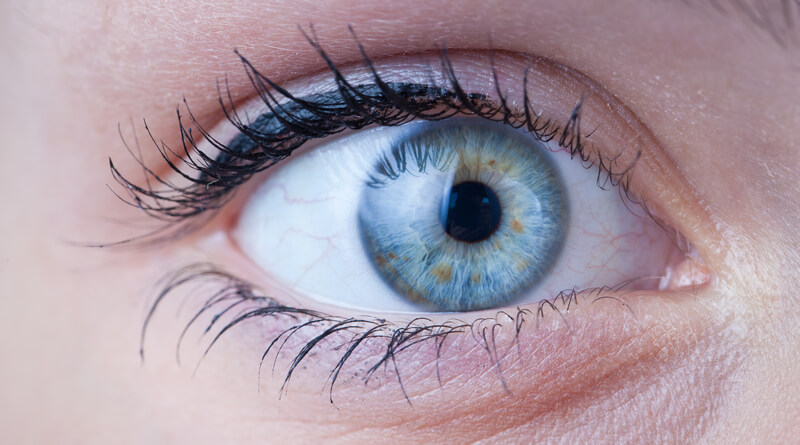
Patient Photos Should be Captured During Registration
Despite the rising demand for biometric patient identification to improve patient identification and increase safety, not all solutions are created equal. Healthcare organizations that invest in unilateral biometric patient identification solutions quickly discover that they do not have the ability to easily and automatically capture the patient photo during registration and subsequent visits. This is unfortunate as the photo plays an important role in patient safety and in driving additional value throughout the ecosystem.
In addition, capturing the patient photo with a web camera during initial registration is not enough. This method often produces very poor quality photos, adds an extra step to the process, and the photos cannot be relied upon for other potential uses, such as facial recognition to verify patient identities during remote encounters.
One important differentiator that should be considered when researching a biometric ID solution is whether or not it offers the ability to capture a high-quality patient photo and recognize the patient in a single step. Why?
- Patient photos are proven to reduce medical errors.
- Respected, influential healthcare organizations recommend including patient photos with their medical record.
- Patient photos increase patient safety.
- Photos can be used as a second credential for multi-factor patient authentication.
- The photo serves as a visual reminder to the provider, thereby enhancing caregiver communication with the patient.
- High-quality patient photos allow healthcare providers to leverage facial recognition for accurate patient ID when patient’s access PHI or services in non-traditional settings such as mHealth apps, patient portals, and telemedicine. This enables a holistic approach to establishing accurate patient ID because it addresses all points along the care continuum instead of a narrow approach that only covers patient ID at the point of service in a brick and mortar setting.
- In areas like the ED where time is critical, utilizing a web camera and adding an extra step in the workflow is impractical and inefficient.
Criteria that Defines an Effective Biometric Patient ID Solution
In addition to the points mentioned above and the standard questions that should be asked when researching the adoption of a biometric patient ID solution, we recommend that healthcare providers seriously consider the unique value of a platform like RightPatient® that seamlessly captures patient photos and identifies patients in a single step during registration, subsequent visits to a medical facility, and other touchpoints along the care continuum. This establishes a concrete, two-factor audit trail of patient visit activity and identity assurance.
Verify that the biometric patient ID solution offers the following patient photo capture features:
- Convenience – Is the patient photo capture process easy and convenient for patients and staff? Photo capture should happen simultaneously with capturing their biometric credentials and should be fast. Otherwise, you run into delays and registration roadblocks in areas like the emergency room where time is of the essence.
- Seamless integration and functionality – Patient identification and photo capture should be a seamless part of EHR workflow and not require staff to sign in and out of applications or constantly toggle between applications.
- Affordability – Biometric patient ID platforms that offer simultaneous photo capture should be flexible and affordable and offer a software-as-a-service (SaaS) model option.
Conclusion
Capturing patient photos to increase safety and reduce medical costs is not a new concept in healthcare, yet it has failed to become mainstream compared to other industries. In fact, according to a recent report from the ECRI, despite the proven research that photos increase safety and engagement, only 20% of existing providers currently use patient photos. 20%! Think about that in the context of other industries that have used customer photos as part of their routine identification security protocols for years: membership management (e.g. gyms, fitness clubs), banking and finance, retail, education, government — the list is long.
If other industries have relied on the use of photos to augment identification accuracy, why is healthcare so far behind the curve? It seems as if healthcare market conditions and current and future initiatives to improve delivery, achieve better outcomes, perfect individual and population health, and reduce the cost of care are setting the stage for technology that can quickly and seamlessly capture patient photos as part of the identification process. The question is, are you investing in the right solution to harness this power?
 Michael Trader is President and Co-Founder of RightPatient®. Michael is responsible for overseeing business development and marketing activities, government outreach, and for providing senior leadership on business and policy issues.
Michael Trader is President and Co-Founder of RightPatient®. Michael is responsible for overseeing business development and marketing activities, government outreach, and for providing senior leadership on business and policy issues.











 Brad Marshall is an Enterprise Development Consultant with RightPatient®. With several years of experience implementing both large and small scale biometric patient identification projects in healthcare, Brad works closely with key hospital executives and front line staff to ensure project success.
Brad Marshall is an Enterprise Development Consultant with RightPatient®. With several years of experience implementing both large and small scale biometric patient identification projects in healthcare, Brad works closely with key hospital executives and front line staff to ensure project success.







