Telemedicine/Telehealth is growing….fast
It’s difficult to call telemedicine the shiny new object in healthcare, mostly because it’s origin can be traced back to the first half of the 20th century. In fact, the first people to use video communication for medical purposes were clinicians at the University of Nebraska who in 1959 established a two-way television setup to transmit information to medical students across campus, and five years later linked with a state hospital to perform video consultations. (source: http://evisit.com/history-of-telemedicine/)

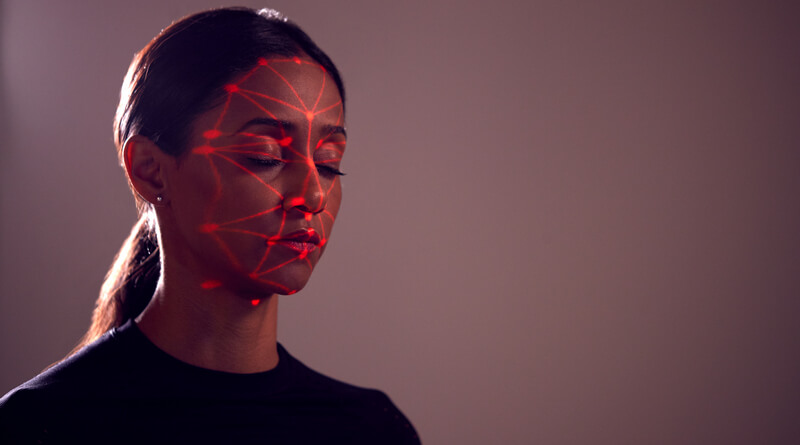
The rising use of telemedicine services in healthcare demands a more holistic approach to accurate patient identification.
Since then, telemedicine has rapidly evolved as a trusted source of care, particularly for patients living in rural areas who traditionally have limited access to healthcare, and the industry is expected to reach 7 million patients worldwide by 2018, fueling an 18 percent growth rate by 2020. This is good news for a wide swath of key players in healthcare, especially providers who are already laser focused on advancing healthcare’s “triple aim” – improving the patient experience, improving population health, and reducing the per capita cost of care, plus telemedicine has proven to be a strong tool to increase patient engagement. Patients stand to benefit handsomely from advances in telemedicine too for its convenience and accessibility, quickly latching on to the “care when and where you want it” mantra of the technology.
Yet, for all it’s convenience and increased accessibility, healthcare providers should take caution on procedures in place to identify patient identities prior to administering telemedicine services. Advances in telemedicine combined with an influx of newly insured patients under The Affordable Care Act have undoubtedly spawned opportunities for patients to commit fraud by stealing or swapping identities to receive services they aren’t eligible for. Undoubtedly the issue of limited reimbursement continues to be a major barrier to the expansion of telehealth — shouldn’t providers pay more attention to adopting technology that establishes a concrete and indisputable audit trail for telemedicine services?
What can telemedicine healthcare providers do to increase patient identification accuracy and adopt a strategy that has the capability to address the need to ensure a patient is who they claim to be?
Telemedicine patient ID laws murky, differ from state to state
As is the case with administering a lot of other digital health tools in healthcare, rules and regulations are fragmented and differ from state to state. Some states like Maryland, Virginia, and New Mexicohave laws and regulations that facilitate the greater use of telemedicineyet others such as Texas are actively seeking to pass laws that restrict telemedicine services to only those patients who have previously seen a doctor.
Regulating telemedicine is a tricky endeavor in healthcare. Most healthcare providers (especially those in medically underserved, rural communities) want to see the expansion of telemedicine because of the potential gains in individual and population health plus increasing the convenience of healthcare delivery helps build patient loyalty and speciality physician access. Think about how much good will is built with chronically ill patients who don’t have to make a painful journey to the doctor’s office to receive care!
However, the potential risks of fraud and medical identity theft by telemedicine patients because of the apparent ease of assuming another person’s identity threatens to jeopardize patient safety and compromise patient data integrity which is essential to maintain in an era of increased interoperability and data sharing. Perhaps Alison Diana, formerly of Information Week, summed it up best by saying: “With multiple organizations providing their well-meaning suggestions, states following their own rules, and insurers taking various strategies, telehealth adoption is hampered by fear, uncertainty, and doubt.”
What’s clear is that telemedicine is yet another tool in a provider’s toolbox that deserves the same patient identification scrutiny and caution given to a face-to-face encounter. Health data security is an issue in healthcare that has evolved beyond brick and mortar identification scenarios and expanded to any point along the care continuum where a patient has access to data or care services. As President and CEO Russell Branzell and Board Chair Charles Christian of CHIME said, “As data exchange increases among providers, patient data matching errors and mismatches will become exponentially more dangerous and costly.” (source: http://www.globalmed.com/telehealthanswers/telehealth-data-security-and-a-national-patient-id/)
With the number of employers increasing employee telemedicine service offerings and the number of people now eligible for these services now estimated to be in the tens of millions, the healthcare industry has a vested interest to ensure 100% accurate patient identification.
Holistic patient identification is the new norm
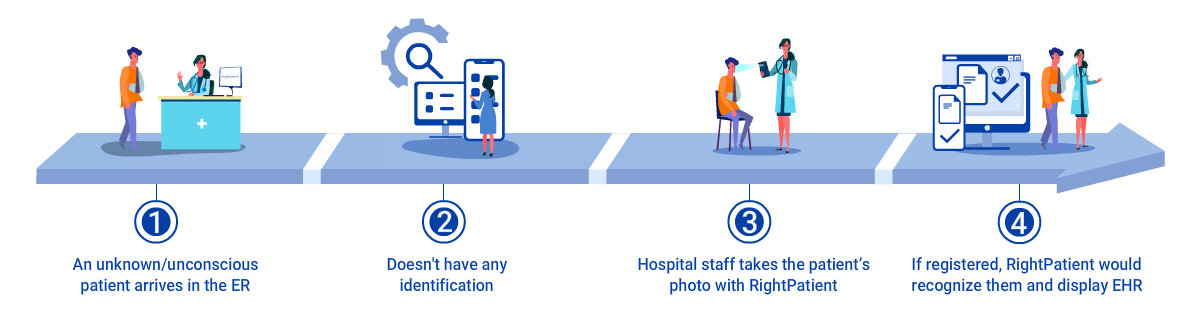
The digital age of medicine has created a host of new patient touchpoints along the care continuum that require healthcare providers to reassess their patient identification policies to ensure that patients are safe, treatment is accurate, protected health information is attributed to the correct medical record and fraud does not cause medical errors that could increase provider liabilities. The conundrum for healthcare providers is identifying a patient identification technology that has the capability to provide accurate patient identification no matter where a patient is along that care continuum and can flexibly be used at ANY touchpoint, regardless if it’s virtual or physical.
What’s interesting about the explosion of these new patient touchpoints and accessibility is that provider focus (justifiably) is usually targeted on technology, compliance, and reimbursement — all important components to ensure success. For example, articles prognosticating about what telemedicine needs to succeed rarely address adopting stricter patient identification technology to protect both patient and provider. However, our field research demonstrates that healthcare providers are increasingly paying closer attention to perhaps the most essential element of any digital health tool, the absolute necessity of ensuring accurate patient identification prior to administering care.
When it comes to accurate patient identification, telemedicine should not be treated any differently than, say, access to a patient portal or a physical trip to a doctor’s office. Holistic patient identification accuracy protocols that have the flexibility to be used in different capacities but ultimately to achieve the same purpose — ensuring patient identification accuracy and patient data integrity no matter when or where a patient seeks access to medical information or services.
Photo biometrics a perfect fit for patient ID in telemedicine
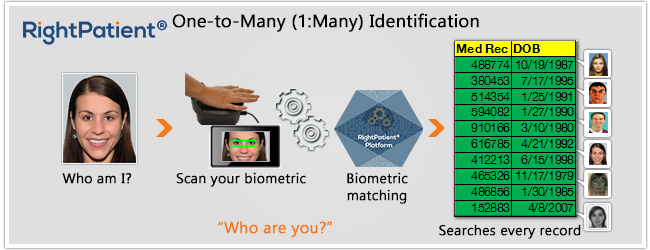
One patient identification technology surging to meet the demand for holistic patient identification in healthcare is biometrics. The use of biometrics for accurate patient identification in healthcare offers immediate, sustainable benefits (increases in patient safety, reductions of duplicate medical records, elimination of fraud) but what often goes unnoticed are broader, tangential advantages that can be applied to new patient touchpoints along the care continuum.
For example, a healthcare provider using photo biometrics for patient identification in healthcare can ensure accurate patient identification at the point of service then have the ability to verify that same patient’s identity through a portal, or prior to a telemedicine session using facial recognition. Hospital re-admission reduction provides an excellent example of a tangential benefit biometrics delivers to the healthcare industry. By ensuring the accuracy of a patient’s identity during a home health visit or telemedicine session (key components to reduce re-admits), healthcare providers can administer accurate, timely patient care that helps reduce the possibility of a re-admission which significantly adds to the cost of care and can result in Medicare reimbursement reductions.
Biometrics for patient identification offers another distinct advantage to telemedicine — an indisputable audit trail. Healthcare providers can rest assured that they now have a concrete list showing which patient accessed telemedicine services and what day and time they received the services. In this era of shifting regulations and evolving legislation, healthcare providers who implement photo biometrics for patient identification are at a distinct advantage over those that may rely on more antiquated methods to verify patient identities.
Although the use of photo biometrics for holistic patient identification across the care continuum is a new concept in healthcare, more providers understand its value and are exploring the use of this technology.
Is patient identification for telemedicine services a concern for you? What specific challenges do you face?
Leave us a comment below!


















 Michael Trader is President and Co-Founder of RightPatient®. Michael is responsible for overseeing business development and marketing activities, government outreach, and for providing senior leadership on business and policy issues.
Michael Trader is President and Co-Founder of RightPatient®. Michael is responsible for overseeing business development and marketing activities, government outreach, and for providing senior leadership on business and policy issues.