Biometric Data Analysis for Chemical Exposure Monitoring

Biometric data has demonstrable advantages in numerous applications and has become practical for medical professionals due to its convenience and accuracy. While this field is still growing, its modern uses have benefits and drawbacks. Here’s how the medical field uses biometric data for chemical exposure monitoring.
How Can Biometric Data Monitor Chemical Exposure?
Monitoring chemical exposure is crucial in healthcare facilities to protect patients and staff. Cleaning products, sterilizers and gases are only some components people encounter inside a hospital or medical practice, emphasizing compliance with indoor air quality regulations to comply with workplace safety laws.
Fortunately, biometric data has become helpful in monitoring this exposure and improving safety. The primary way medical professionals can accomplish this is through the Internet of Things (IoT) devices, which track patients and staff inside a healthcare facility and use historical data to identify trends. Therefore, healthcare facilities can keep all occupants safe and sound.
The vast number of tools available to researchers has permitted tracking chemical exposure through sensors. Here are some of the ways experts can monitor patients using biometric data:
-
Heart rate monitors: Heart rate monitors are an excellent way to track chemical exposure through biometrics by alerting when it causes a patient’s heart rate to fluctuate.
-
Blood pressure monitors: Blood pressure monitors are integral to biometrics because they demonstrate how exposure has affected a patient’s vitals.
-
Skin temperature detectors: A person’s body is prone to temperature changes when exposed to chemicals, making skin temperature monitoring devices useful for displaying the difference.
-
Breathalyzers: When the user operates a breathalyzer, they can see the concentration of chemicals. For example, pairing the breathalyzer with a pulse oximeter paints a clearer picture of what the patient has inhaled by examining their blood oxygen saturation.
What Benefits Does Biometric Data Bring for Medical Professionals?
Considering its efficiency and accuracy, biometric data is the future for healthcare facilities. Here are the benefits medical professionals get when using it for chemical exposure monitoring.
Risk Detection
Humans have become better at detecting diseases and illnesses, but biometric data closes knowledge gaps with advanced technologies. These devices use historical data to create baseline measurements and quickly alert medical professionals when deviations occur, giving them a crucial advantage when every minute matters.
Convenience
Biometric data is typically faster, more accurate and more convenient for the patients. Crowded healthcare facilities in recent years have emphasized the need for patient satisfaction and improved health outcomes. Using this information for chemical exposure monitoring is handy because it’s minimally or non-invasive while providing individualized care for each patient.
Regulatory Compliance
Exposure could derive from a deliberate attack, such as an unleashed chemical intending to harm those inside a crowded building. The symptoms might not initially be evident, so using biometric data analysis makes risk detection and compliance easier.
A facility may be required to comply with CFATS — a Department of Homeland Security program. This division regulates security at high-risk chemical facilities, so protecting staff and all occupants is essential.
What Are the Challenges of Using Biometric Data for Medical Professionals?
While it has positives, biometric data also presents these challenges for medical professionals.
Security
Biometric technology has rapidly evolved in the medical field, but cybersecurity is a significant threat to healthcare facilities and patients. Hospitals are a frequent target for cyberattacks due to the financial records and intellectual property each facility owns. The increased use of biometric data emphasizes security to protect patients as electronic usage rises in healthcare facilities. Thieves seeking sensitive data may use it for insurance fraud or identity theft.
Ethics
Biometric data is crucial to understanding diseases and chemical exposure in a healthcare facility but can lead to privacy concerns for the patient. While security threats are the most significant fear, compromised privacy can derive from the health care facility.
Ethically handling patient information is crucial for medical professionals — for example, a facility could share this data with a third party without the patient’s permission. Hospitals and other healthcare organizations must be honest with their patients about how they’ll use their biometrics.
Limitations
Another problem with biometric data derives from the technology itself. These devices increase accuracy using historical data, statistics and machine learning techniques but are still fallible.
Medical professionals may become wary of tools that malfunction or become less accurate due to wear and tear. Additional limitations may stem from the costs associated with advanced technologies, thus inhibiting healthcare facilities with smaller budgets.
Using Biometric Data for Chemical Exposure Monitoring
While medical technology continues to evolve, biometric data is among the chief innovations in medical facilities. It has demonstrated abilities to detect risks and improve patient care. Employing this practice for chemical exposure monitoring has limitations, but research shows it has positively affected health outcomes.



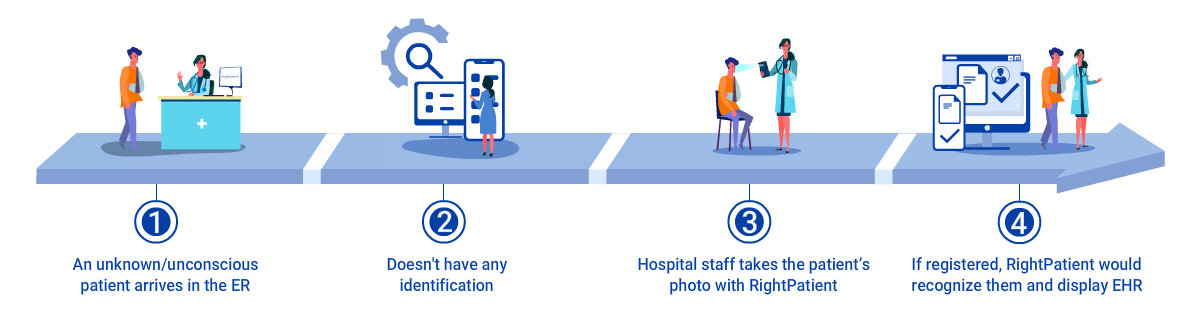
 Michael Trader is President and Co-Founder of RightPatient®. Michael is responsible for overseeing business development and marketing activities, government outreach, and for providing senior leadership on business and policy issues.
Michael Trader is President and Co-Founder of RightPatient®. Michael is responsible for overseeing business development and marketing activities, government outreach, and for providing senior leadership on business and policy issues.