How RightPatient Prevents Chart Corrections in Epic and Other EHRs

I’ve visited enough of our customers to know that hospital emergency rooms and free-standing EDs can sometimes be chaotic environments. Unlike most outpatient registration areas, patients who arrive to the ED do not have scheduled appointments and often go through a triage process with a nurse where they are “arrived” within the electronic health record (EHR) system. This is essentially a quick registration that begins the documentation of a patient’s visit information on his/her medical record. Unfortunately, this process often results in what are known as chart corrections.

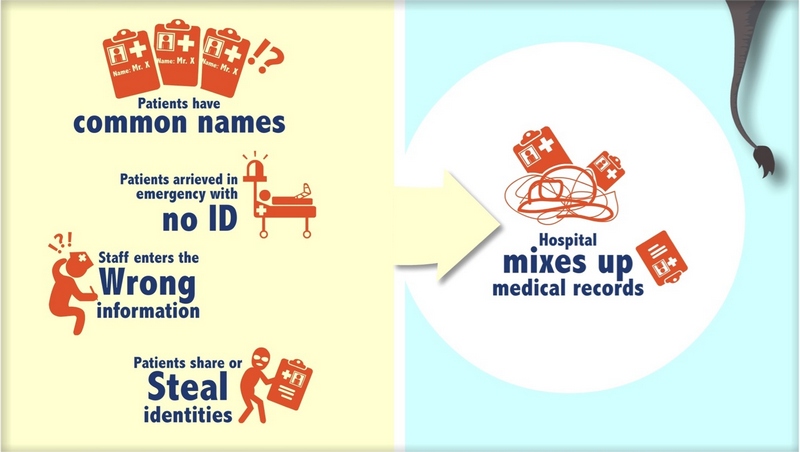
As one might imagine, a clinician’s primary focus is on the health and safety of the patient. Nurses that triage patients are trying to enter patients into the EHR system so they can receive the appropriate care as quickly as possible. Unfortunately, data entry errors during this process are commonplace. For example, EHR system users may create a “John Doe” or “Jane Doe” medical record if they cannot properly identify the patient. Or, users may mistakenly select the wrong record because it shares a similar name with the patient in need of care.
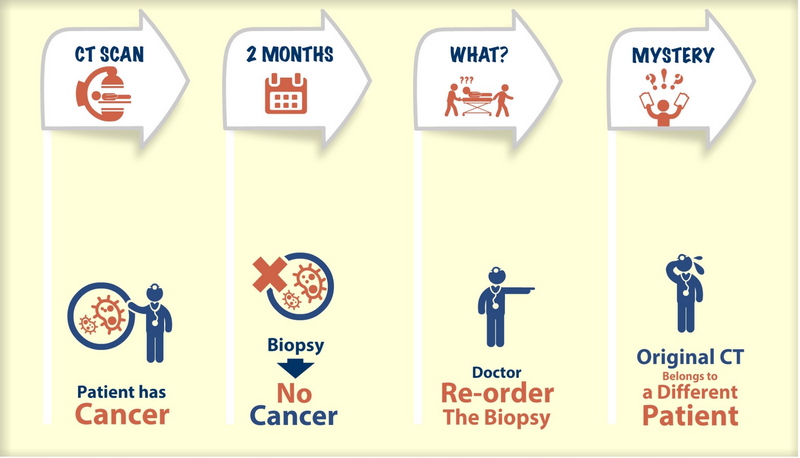
When EHR users select the wrong patient medical record, all subsequent information pertaining to that visit is entered into that record (sometimes referred to as a medical record “overlay”). This is a data integrity failure and results in data entry errors that need to be resolved with a chart correction. So, a chart correction in the Epic EHR or other EHR systems is the process of fixing a “wrong chart entry” or overlay record that was caused by a patient identification error.
Wrong patient, wrong record data integrity failures within the EHR system can have disastrous consequences. At best, the healthcare provider must spend internal Health Information Management (HIM) resources to perform chart corrections and resolve medical record overlays, costing $60-$100 per hour for an average of 200 hours per overlay record. At worst, wrong patient errors can affect clinical decision making, patient safety, quality of care, and patient lives. This is why organizations like AHIMA have strongly advocated safeguards that healthcare providers can use to prevent medical record mix-ups, improve data integrity, and reduce the risk of adverse events.
RightPatient is the ideal safeguard to prevent wrong patient medical record errors and chart corrections within Epic and other EHR systems. The AI platform uses cognitive vision to instantly recognize patients when their photo is captured and automatically retrieve the correct medical record. This becomes a seamless module within EHR system workflows so there is no disruption to users.
Customers like University Health Care System in Augusta, GA are effectively using RightPatient to reduce chart corrections in Epic. In fact, UH saw a 30% reduction in Epic chart corrections within months after implementing RightPatient.
Healthcare providers using RightPatient to capture patient photos significantly reduce their risk of data integrity failures. This enhances patient safety and health outcomes while reducing costs – important goals in the age of population health and value-based care.