Takeaways from the 2015 NE NAHAM Regional Conference – “Improving the Patient Experience”


David Cuberos, Enterprise Sales consultant with RightPatient®, poses with Bryan Marcotte from Baystate Health, winner of the gift card door prize at the 2015 NE NAHAM regional conference.
The following guest post was written by David Cuberos, Enterprise Sales Consultant with RightPatient®
The time that we spend meeting with patient access professionals in the field is important to us. It’s an opportunity for our team to better understand core patient access functions/workflow and how these critical front line staffers help mold the patient experience as a first point of contact in what can often be a long, complex journey through the healthcare system. Our strong support for the National Association of Healthcare Access Management (NAHAM) and their regional chapters is a key relationship — instrumental to our product and service design and the ability for us as healthcare software vendors to deliver a solution that meets the dynamic needs of these healthcare professionals and moves the patient safety needle in a positive direction.
Last week, we had the opportunity to meet with patient access professionals from the northeast region of the U.S. to discuss the patient access professionals’ impact on the patient experience. We learned a lot about challenges faced by patient access staff, how it impacts workflow, and what new technology solutions are available to help meet the shifting and often complex demands of this position.
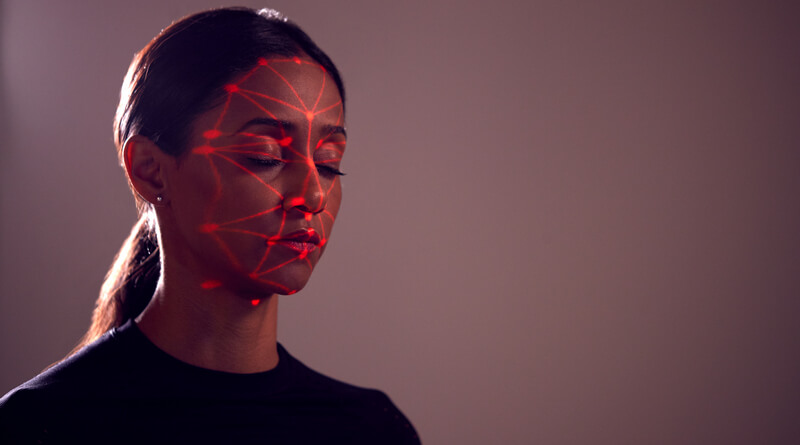
We also had the opportunity to discuss the ongoing conundrum of achieving accurate patient identification with show attendees and display our biometric patient identification solution that helps to increase patient safety and eliminate duplicate medical records/overlays and prevent medical identity theft and healthcare fraud. This was an ideal environment for us to not only help educate attendees on the value of implementing a patient identification solution, but it also provided us the opportunity to clear up misunderstandings about how this technology operates in a healthcare setting. As we do at all events, we learned a great deal about what types of questions healthcare professionals have about this technology and walked away with some key takeaways:
1. Retinal scanning and iris recognition are two different biometric technologies: This is a recurring misunderstanding we consistently see wherever we go. Due to the fact that both retinal scanning and iris recognition use the human eye for identification, most people believe that the technology is the same. In fact, the two are very different – explained in this blog post we wrote that breaks down the differences between iris recognition and retinal scanning.
2. Patient acceptance of iris recognition is extremely high: Some believe that using the iris as a unique identification credential can invoke patient trepidation to register their biometrics as a way to protect their identity and ensure accurate treatment throughout the care continuum. However, when healthcare staff observes the iris camera in person, they realize that it is perhaps the least invasive biometric modality because it simply takes a high-resolution digital photograph of the patient and can identify them in less than three seconds. Our field research supports patient acceptance of iris recognition for identification, with over a 99% acceptance rate.
3. Proper due diligence of biometric patient ID vendors is critical: Did you know that not all biometric matching types support the elimination of duplicate medical records or have the ability to prevent medical identity theft and healthcare fraud in real-time? Are you concerned about implementing a contact dependent biometric modality for patient identification that may jeopardize hospital infection control policies or require additional investments in a cleaning solution or wipes after each use? Does a biometric identification system seamlessly integrate with your electronic health record system to accurately authenticate patients from any touchpoint along the care continuum? Does your biometric patient identification solution have the ability to secure remote access to protected health information (PHI) from patient portals and/or mHealth apps?
These are all important to ask when evaluating biometric patient identification vendors but our experience is that many hospitals aren’t asking the right questions.
4. Hospital resources to resolving duplicate medical records are staggering: We continue to be amazed at the number of hospital staff dedicated to resolving duplicate medical records. In fact we spoke with a few attendees who mentioned that they have “teams of people” dealing with duplicate medical record clean-up. Although we can’t understate enough the importance of maintaining clean data, we have longed believed that implementation of modern patient identification technologies that have the ability to not only clean a master patient index (MPI), but sustain the integrity of the data moving forward. The key to preventing duplicate medical records is implementation of technology that can accurately identify patients no matter where they are along the care continuum.
5. Patient experience can be boosted through the use of biometric patient identification technology: Patients pay close attention to their experience at a medical facility. Patient knowledge of the negative effects of duplicate medical records and medical identity theft has increased their empowerment to seek services at facilities where their identities are protected. Implementing a biometric patient identification solution to protect patient identities invokes the emotion that medical facilities care about safeguarding patient safety and privacy.
Understanding how to improve the patient experience in healthcare requires careful examination of processes and workflow that bring convenience and demonstrate a genuine interest in protecting patient identities. We continue in our mission to provide the most comprehensive and holistic patient identification solutions available to help improve the patient experience in healthcare.
A special shout out to Bryan Marcotte from Baystate Health as the winner of the gift card door prize. Congratulations Bryan!
How can we help you to improve the patient experience at your medical facility?
 David Cuberos is an Enterprise Sales Consultant with RightPatient® helping hospitals and healthcare organizations realize the benefits of implementing biometrics for patient identification to; increase patient safety, eliminate duplicate medical records and overlays, and prevent medical identity theft and healthcare fraud.
David Cuberos is an Enterprise Sales Consultant with RightPatient® helping hospitals and healthcare organizations realize the benefits of implementing biometrics for patient identification to; increase patient safety, eliminate duplicate medical records and overlays, and prevent medical identity theft and healthcare fraud.











 Michael Trader is President and Co-Founder of RightPatient®. Michael is responsible for overseeing business development and marketing activities, government outreach, and for providing senior leadership on business and policy issues.
Michael Trader is President and Co-Founder of RightPatient®. Michael is responsible for overseeing business development and marketing activities, government outreach, and for providing senior leadership on business and policy issues.


