Improving Patient Safety in Hospitals as They Reopen Post-COVID-19

To say that the coronavirus pandemic will change the world is an understatement. It can never be stressed enough as to how much it has and will continue to impact our lives. After lockdowns were implemented for months to reduce the cases of infections, states are opening up slowly with precautions still in place. The US healthcare system is no exception – some providers are planning to open up while shuttered hospitals are planning to reopen due to the coronavirus. With all that in mind, one issue must have the highest priority now – improving patient safety in hospitals. This article will talk about some ways in which hospitals can reopen safely along with tools that can help them do that.

Improving patient safety in hospitals – some strategies
Come up with a plan
As the US is in a very delicate situation right now, it can only be helped if the providers reopen safely and treat the patients successfully, and all of this starts with an effective plan. Plan the important days accordingly, especially the reopening day. It is wise to take it slowly and reopen in phases rather than opening a hospital all at once, but more on that later. Make an inventory of all the necessary tools and materials at hand that are required for protecting and serving patients, especially PPE. Reordering might be required, so ensure that it is done well in advance to reduce disruptions while providing healthcare services. Also, if not already in place, plans must be made on how to deal with patients or employees with COVID-19 on the premises. This will be the new normal for quite some time, so planning for such scenarios ahead will be beneficial.
Open in phases
While many are already adopting this strategy, it is still worth mentioning why it is important. Opening in phases can help detect which areas of the hospital still need to be addressed, if required, and can be done so easily. Moreover, this will also help to accommodate employees on alternate days—reducing contact and risk of contracting the virus. It will give an overview of the problems and opportunities and give everyone time to come up with solutions for dealing with them.
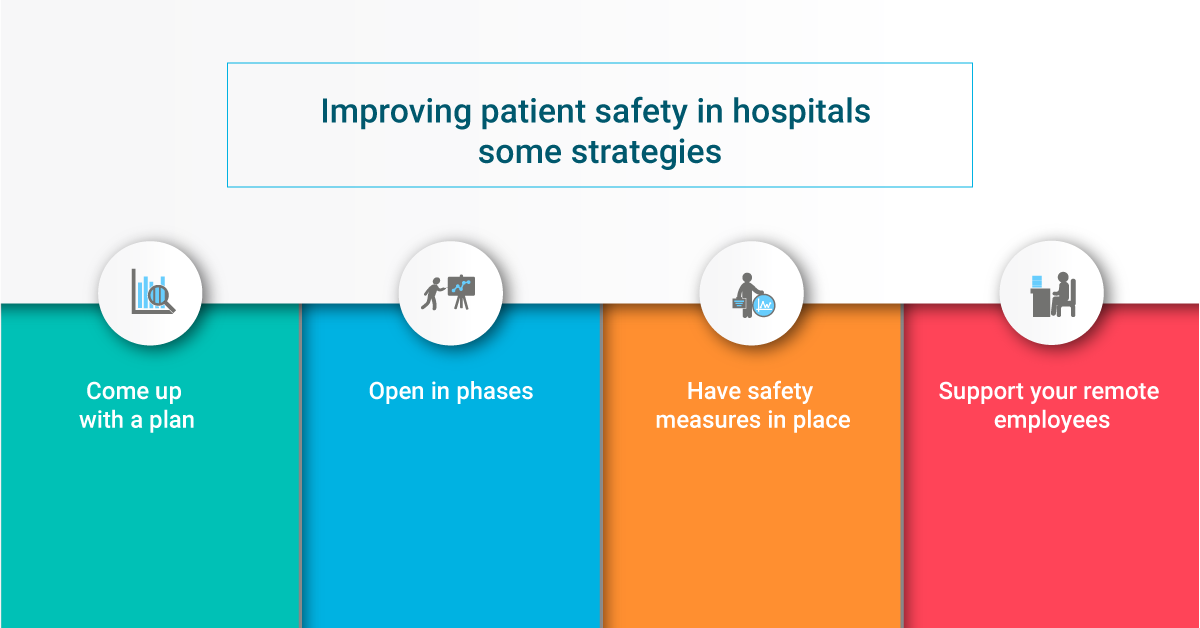
Have safety measures in place
Even though there will be immense pressure on health systems, they need to ensure that patients are not overflowing all the time to maintain social distancing to some extent. For starters, hospitals need to ensure that patients are segregated to keep the ones potentially infected with COVID-19 separated from the ones that do not have it, improving patient safety in hospitals.
Ensuring that everyone on the premises is wearing PPE is a must. Also, ensuring that everyone is maintaining distance, whether employees or patients, is quite important—rearranging layouts to ensure that distance is maintained can help. Also, ensure that minimal contact is required, especially in places like the EDs, since that is where most cases will be present.
If employees exhibit any of the symptoms of COVID-19, encourage them to take leaves, as keeping them in the workplace will only make matters worse.
Support your remote employees
Telehealth has been one of the most useful tools during the pandemic, and it will be used thoroughly in the future as well. Ensure that the remote physicians are properly accessing and using the tools required for telehealth so that the patients who can be served via telehealth do not need to come to the premises, reducing the chances of infections.
However, other than physicians, other employees are also working from home either on alternate days or for the foreseeable future. This is being done to reduce infection rates by practicing social distancing. Ensure that the employees are receiving enough support to carry out their tasks to provide better healthcare outcomes, improving patient safety in hospitals in the process.

Use solutions to reduce infection rates and administrative burden
The US healthcare system is inundated with a plethora of problems. While they are not new and have solutions to mitigate them, many are still not using these solutions; thus, they are still suffering from the issues. With the coronavirus pandemic in mind, it is high time that these problems are addressed by healthcare providers.
First off, let’s look into HIPAA compliance issues. Even though HIPAA penalties have been relaxed, for now, there are still many rules and regulations that need to be followed. While healthcare providers are already working around the clock to serve patients, ensuring HIPAA compliance can be a huge challenge, given the situation. Using solutions like HIPAAReady can reduce the administrative burden and simplify compliance management. With internal auditing, training management, and keeping HIPAA information in a centralized location, HIPAAReady is already an attractive HIPAA compliance software to mitigate HIPAA compliance issues.
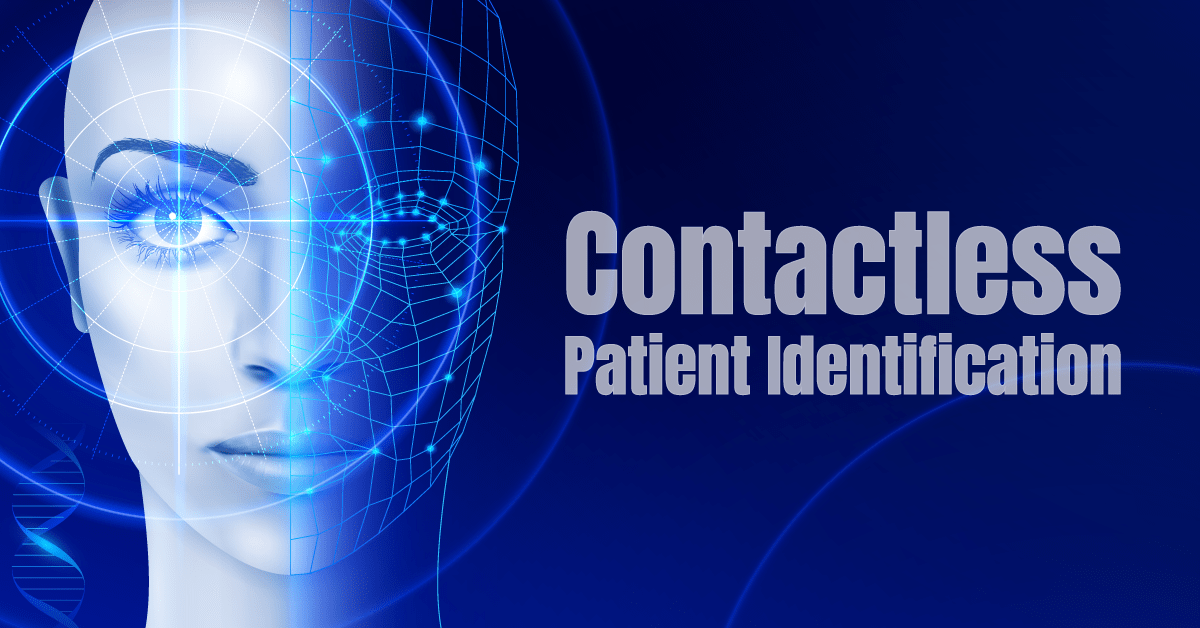
Patient identification errors, on the other hand, have been haunting providers for decades. It has been an impediment to improving patient safety in hospitals. While many have been using different identification solutions like fingerprint scanning and palm-vein scanning, the pandemic will render these modalities obsolete. Earlier, infection control issues were only a headache of the providers, but the pandemic will make patients reluctant to use any identification solution requiring touch. Fortunately, there are already touchless biometric patient identification solutions available with RightPatient being the most appropriate one. After registration, the platform requires the patient to only look at the camera. The platform matches it with the registered template and retrieves the accurate medical record within seconds. All of these require no physical contact from the patient, enhancing patient safety as well as acceptance.
Providers like Terrebonne General Medical Center and Community Medical Centers are already using RightPatient and have chosen it as there are no infection control issues surrounding the platform like other modalities, making it an ideal patient identification solution in a post-COVID-19 world. When providers are losing millions due to the pandemic, deploy RightPatient and mitigate losses by ensuring touchless patient identification, preventing medical identity theft, and reducing denied claims.