5 Most Significant Tech Trends In Health Information Management (HIM)

The following guest post on trends in Health Information Management (HIM) was submitted by Broadwater.
The sheer power of technology has paved the way for the development of the latest tech systems in Healthcare Information Management (HIM). We have witnessed how the Electronic health systems have gone through many changes over the past few years. These advanced breakthroughs are deployed with a goal to enhance the efficiency of healthcare information management systems, and to promote something that will allow health care facilities to deliver the best possible treatment and care to every patient. Let’s walk through the 5 biggest technological trends that embark a great contribution on modern Healthcare Information Management.

Learn about new technologies positively impacting Health Information Management (HIM) departments in healthcare.
Mobile Access
Imagine this: a physician had to be physically present in the office in order to examine a patients’ case. Gone are those days. Thanks to the rise of mobile devices like smartphones and tablets; more doctors are now able to work remotely, conveniently storing healthcare records over a cloud. Traditional IT infrastructure is now being replaced by cloud based azure windows virtual desktop with the help of daas providers which makes it easy for doctors to keep an eye on their office by sitting at home. This way, they can easily access pertinent information regardless of where they are, through the use of mobile devices. This is especially useful during medical emergencies, where a patient can receive quick and efficient diagnosis and treatment, wherever their doctors are.
Electronic Health Records
While Electronic Medical Records (EMRs) contain patient information about diagnosis and treatment, Electronic Health Records (EHRs) provide a more detailed view of the medical story of the patient, including allergies, previous medications, immunization records, and other relevant data. Through electronic storage of the patient information, health care centers do not only save on paper files, but it also provides a much easier and more convenient access by the health care provider. Thanks to its reliable searchable database that makes finding Healthcare Information Management simpler and more efficient, thus improving the way healthcare services are provided.
Virtual Conferencing
To provide a top-line healthcare service, doctors have to consult with peers. And obtaining a second opinion on patients’ medical records from a peer specialist is a smart way to ensure that patients receive proper diagnosis and treatment. At present, video conferencing makes way for a much easier and more effective consultation. Doctors are now able to speak with other experts around the world in the comfort of their own homes or offices.
Unified Communication Platform
While video conferencing is a great choice to seek outside help, unified communication systems benefit Healthcare Information Management within a medical facility. When multiple nurses and doctors are working on the same patient, it is necessary that every bit of information should be up to date and readily available for everyone’s access. This means that an open line of communication is the key to efficient healthcare service. With a unified communication system, information can be easily updated though text, email, micro-blogging and IM. Most importantly, every member of the team can readily view the thread.
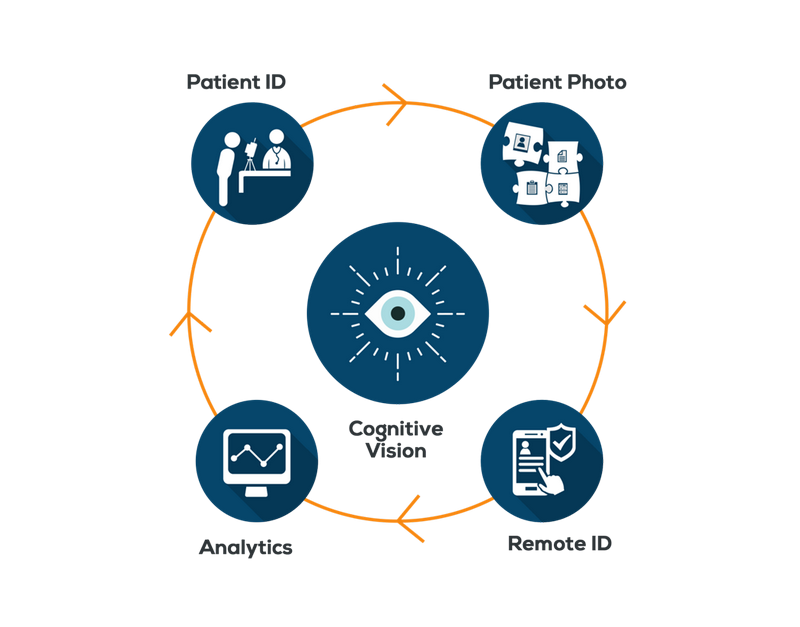
Privacy and Security
One of the most pressing concerns regarding Healthcare Information Management in an online setting is the risks of security issues. In today’s world where every bit of information can be accessed using any device and from any location, it is paramount that healthcare information management teams should take all the essential measures to prevent any issues. Privacy and security can be reinforced thorough password protection, and a strict verification process. The management should have a keen eye for malware, viruses and other attacks that can pose threats to the integrity of the patient information.
Medical science gets more and more cutting-edge in terms of technological development as the years pass by. A high-performing medical tool or a new procedure can make the difference between life and death. Be assured without a doubt there are tremendous changes that await us in the field of Health Information Management.