HIMSS 2019 – Interoperability Showcase; What Is the Foundation of Interoperability?


HIMSS19 Global Conference & Exhibition, Orlando, FL
On the last day before leaving, I decided to stop by the interoperability pavilion at HIMSS – this was one of the busiest and well-presented parts of the show. The section, showcased by the VA (US Veteran Administration), was very extravagant – you usually see such displays from any of the federal government agencies only in Washington D.C. The VA is definitely a front-runner in interoperability – they are the first one to initiate the blue button program to share medical records. The jam-packed area with vendors and exuberant people from all corners of the HealthCare industry clearly shows the importance of the mission. As I was snapping a selfie, Andy Pincsak from Phillips Health jumped in & joined my memory lane – I thought it was a very nice and friendly gesture! Why can’t we all be like that with each other?

Snapping a selfie with Andy Pincsak from Phillips Health
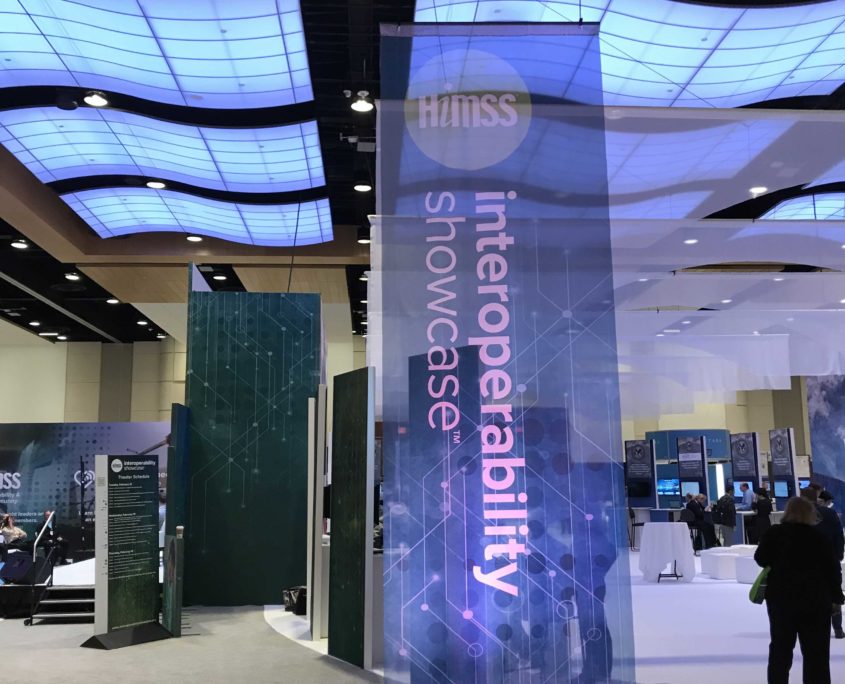
The HIMSS Interoperability Showcase™ was the highest trafficked area of the exhibit floor

Innovative Solutions on the Exhibit Floor
Why Is Interoperability Such a Big Deal?
The fundamental premise of interoperability is to share data between organizations – so a patient can move from provider to provider and his/her data can be seamlessly shared between the providers. This is very serious because an average American with chronic conditions, such as diabetes, sees multiple physicians from various organizations. To orchestrate a meaningful treatment regimen to such patients, it’s imperative that each of these providers has real-time visibility of each patient’s care-cycle. Hence, interoperability is extremely crucial.

Innovation Live brought together startups, accelerators, and other innovative companies to showcase the future of healthcare IT
What’s the Fundamental Flaw in the Healthcare Interoperability Movement?
For interoperability to be successful, the providers must match and identify the patient as they move between the organizations – to be clear, your social security number is the unique identifier. But in healthcare, every organization assigns its own unique numbers to each patient. Therefore, how will organization A notify organization B that John Joe with ID “DX213” is the same “John Doe” with ID “74537”? Currently, this is done using fuzzy match. However, on an average 8% of the time, a patient is registered under a different name – I am serious – this is called a duplicate patient record. Since many people have common names and there is no social security number in their health record, a simple mistyping – usually called fat finger – causes the creation a different record for a patient that already has a record. Therefore, how in the world can all these providers really work in harmony and share data with such a mess? It does not take a rocket scientist to understand these issues. To achieve real interoperability, we need clean and uncorrupted data.

HIMSS Interoperability Showcase
Is There Any Solution Without Using a Social Security Number?
Of course there is. Since we can’t rely on names and names also change, we can easily add patient biometric data with each medical record. Once a patient is tagged with his/her biometrics, they will always be identified with just biometrics. Basically, a patient will just walk into a provider’s office, have their biometrics taken and the system will find the record with biometrics. Now, if all providers are using a photo based system like RightPatient, then the patient can move between whole ecosystems without ever worrying about ending up with corrupted data. Why we are not using our natural identifier to protect our health and implement seamless interoperability?